LASIK Surgery
LASIK (laser-assisted in situ keratomileusis), is the most popular refractive surgical procedure. In this procedure, a laser is used to permanently change the shape of the cornea (the clear covering on the front of the eye) to correct common vision problems such as nearsightedness, farsightedness, astigmatism, and presbyopia. This improves vision and reduces a person's need for glasses or contact lenses.
LASIK uses an excimer laser (an ultraviolet laser) to remove a thin layer of corneal tissue, giving the cornea a new shape, so that light rays are focused clearly on the retina. In the case of a nearsighted person, the goal of LASIK is to flatten the too-steep cornea; with farsighted people, a steeper cornea is desired. LASIK can also correct astigmatism by smoothing an irregular cornea into a more normal shape.
LASIK is an outpatient surgical procedure with no need to stay at the surgery center overnight as it will take 10 to 15 minutes to perform for each eye. The procedure is done while the patient is awake, but the patient may request mild sedation. The only anesthetic used is eye drops that numb the surface of the eye. LASIK can be done on one or both eyes during the same session.
How to Prepare for LASIK Eye Surgery?
Before LASIK eye surgery, the eye surgeon will evaluate the patient’s medical history and perform a full eye examination, including measuring corneal thickness, refraction, corneal mapping, eye pressure, and pupil dilation. Afterward, the surgeon will discuss what to expect during and after the procedure.
On the day of the surgery, eat a light meal before going to the doctor and take all prescribed medications, if any. Do not wear eye makeup, creams, perfumes or lotions on the day before and the day of surgery, or have any bulky hair accessories that will interfere with positioning head under the laser.
Contact lenses shouldn't be worn for at least three days prior to the evaluation. In the case of, rigid gas permeable contact lenses, they should not be worn for at least three weeks before. Patients should arrange for a ride home from the place of surgery, as their vision might be blurry.
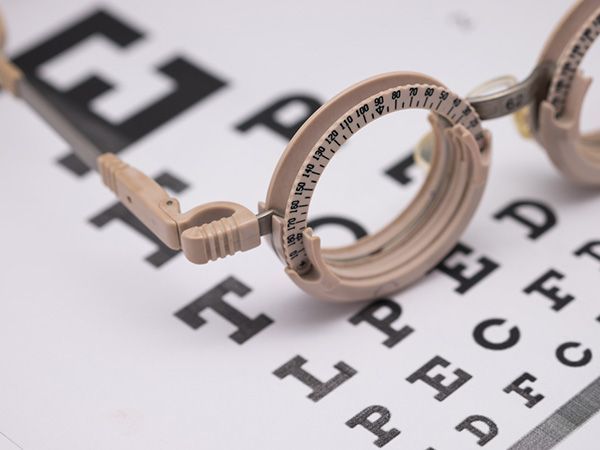
Refraction Test
A refraction test, also called a vision test, is usually performed as a part of a routine eye examination. The purpose of this test is to determine if a person has a refractive error which would then mean the patient would need glasses or contact lenses.
What Is The Normal Value for Refraction Test?
A value of 20/20 is normal (optimum) vision. This means that individuals who have 20/20 vision are able to read letters that are 3/8-inch (1 centimeter) tall from 20 feet (6 meters) away. The normal uncorrected vision (without glasses or contact lenses) refractive error is zero (plano). Individuals who don’t have 20/20 vision, have what is called a refractive error. A refractive error means that the light is not bending properly when it passes through the lens of the eye. The refraction test will tell the doctor what prescription lens should be used in order to have 20/20 vision.
For people over age 40 who have normal distance vision but difficulty with near vision, a refraction test with a small type size is used to determine normal near vision and the correct power of reading glasses.
How Is The Refraction Test Performed?
The test is performed by having the patient seated in a chair that has a special device (called a phoropter or refractor) attached to it. The patient looks through the device and focuses on an eye chart 20 feet (6 meters) away. The device contains lenses of different strengths that can be moved into the patient’s view. The test is performed one eye at a time. If the patient is wearing contact lenses, they should be removed before the test.
In case the final vision is less than 20/20 even with lenses, then there is probably another non-optical problem with the eye. The vision level achieved during the refraction test is called the best-corrected visual acuity (BCVA).
What Are The Causes of Abnormal Refraction Test Results?
Abnormal results may be due to:
Astigmatism (abnormally curved cornea causing blurred vision)
Hyperopia (farsightedness)
Myopia (nearsightedness)
Presbyopia (inability to focus on near objects that develop with age)
Other conditions under which the test may be performed:
Corneal ulcers and infections
Loss of sharp vision due to macular degeneration
Retinal detachment (separation of the light-sensitive membrane (retina) in the back of the eye from its supporting layers)
Retinal vessel occlusion (blockage in a small artery that carries blood to the retina)
Retinitis pigmentosa (an inherited disorder of the retina)
There is an art to refraction and the optometrist will always answer the patient’s questions and as well as discuss their findings. Based on the results of the refraction test, they can determine the amount of myopia, hyperopia or astigmatism.
Amblyopia
Amblyopia, also known as a “lazy eye”, is described as a reduced vision in one eye compared to the other. There are some rare forms of amblyopia that involve both eyes. Amblyopia is the most common cause of partial or total blindness in one eye in children.
The term lazy eye is misleading because the eye is not actually lazy. In fact, it is a developmental problem in the nerve connecting the eye to the brain, affecting the brain’s ability to use both eyes together. It is not a problem in the eye itself, but in the brain which actively ignores the visual input from the misaligned eye, leading to amblyopia in that eye.
In addition to poor visual acuity, people with amblyopia are more prone to having difficulties with depth perception, eye movements related to reading, and visual decision making while driving.
What Are The Causes of Amblyopia?
Amblyopia develops in childhood due to:
Significant differences in the prescription (refractive) status between the two eyes due to nearsightedness, farsightedness or astigmatism;
Constantly misaligned eyes or crossed eyes (strabismus);
An obstruction of vision in early childhood i.e. cataract, ptosis (droopy eyelid)
It is important to note that, because amblyopia is typically a problem of infant vision development, symptoms of the condition can be difficult to detect. Symptoms may include noticeably favoring one eye over the other, an eye turn (either upward-downward outward or inward) or a tendency to bump into objects on one side.
The best way to identify children who are at risk for or already have amblyopia is by performing comprehensive eye examinations.
How Is Amblyopia Treated?
Amblyopia can be treatable at any age, although the earlier the problem is found and treated, the more successful the outcomes tend to be.
Types of Daily Contact Lenses
Wearing contact lenses gives patients the flexibility and freedom to live life to the fullest, without some of the difficulties presented by wearing glasses. Many people who choose contact lenses do so because they don’t like the way that glasses look or feel, or because wearing glasses compromises their ability to perform certain tasks or activities, such as sports or jobs that require the use of safety goggles.
There are lots of different contact lenses to choose from, with two of the most popular being daily disposables and toric lenses.
Disposable Lenses
As their name suggests, these daily contact lenses are disposable. This means that they can and should be discarded at the end of each day rather than re-worn. Disposable lenses do tend to be a little more expensive than some repeat-wear varieties, but the benefits usually outweigh the cost.
Some of the advantages of choosing daily disposable contact lenses include:
You don’t have to clean them, which saves patients a great deal of time and hassle. It also helps save money in terms of the ongoing cost of cleaning solution.
Disposable lenses are also great for people with eye allergies. This is because with ordinary lenses, there’s an opportunity for deposits and microorganisms to build up. With daily disposables, allergens have less chance to attach themselves to the lenses and cause irritation and other allergy symptoms.
You don’t need to schedule regular replacements either, which makes wearing contact lenses easier on your schedule.
Disposable contact lenses are particularly good for people who have busy lives and are likely to cut corners when it comes to caring for their eyes or contacts since there is no cleaning or maintenance required.
Daily disposable contact lenses are available in a wide range of prescriptions, including those for patients with nearsightedness and farsightedness. Your eye doctor will be able to advise you if you are a candidate for disposable contact lenses.
Toric Lenses
Toric contact lenses are recommended for patients who have a refractive eye problem called astigmatism. Patients with astigmatism have corneal abnormalities that cause the refraction of the eye to be different between the vertical and horizontal planes, causing blurred vision and difficulty seeing fine details. Toric contact lenses are shaped in a particular way that creates the different focusing powers needed in each part of the lens to correct your vision. For this reason, it’s essential that Toric lenses are placed into the eyes in the correct position.
Fortunately, manufacturers design Toric lenses with features that help them to stay in place, including:
Thin/thick zones
Creating areas of the lens that are thicker or heavier which helps secure it in position
An area where the bottom of the lens is slightly cut off
To keep them stable, Toric lenses are a little firmer than conventional soft lenses. This means that some patients can find them a little less comfortable, but the superior vision they obtain outweighs this. Your eye doctor will be able to advise you if you are a good candidate for Toric contact lenses and which variety would best suit you.
To find out more about daily contact lenses, speak to our friendly and knowledgeable team.
Keratoconus and Your Treatment Options
Keratoconus is a terrifying diagnosis to those that have experienced it. To compound issues, many patients complain that they had poor initial treatment due to a lack of understanding about the disease. If proper treatment is not achieved, individuals may experience a rapid deterioration in their ability to see. This leads to a reduced quality of life. You can reduce the stress related to a keratoconus diagnosis and increase the benefits of treatment by understanding your treatment options.
Understanding Keratoconus
Keratoconus is an eye disease that causes the cornea to thin and bulge. This bulge generally takes on the appearance of a cone. As light enters the eye, it becomes distorted by the cone causing vision abnormalities.
Modern research is connecting keratoconus with an enzyme imbalance in the cornea. This imbalance leaves the eye susceptible to oxidative free radicals. Keratoconus has also been linked to UV damage, excessive eye rubbing, poorly fitting contacts, and chronic eye irritation.
Treatment Options
While your eye professional will have the best understanding of what treatment option is right for you, we have compiled ten of the most common treatments here.
Corneal Cross-linking (CXL) – There are two different types of this procedure, but they both introduce riboflavin to the cornea in order to strengthen the corneal tissue and stop the bulging from progressing.
Custom Soft Contact Lenses – Soft contacts are generally more comfortable to wear than gas permeable lenses. Recently, some contact companies have been able to create a contact specifically to correct the issues related to mild and moderate cases of keratoconus.
Gas Permeable Contact Lenses – Gas permeable lenses are a hard contact lens that physically forces the eye to adhere to the lens shape. This allows for the correction of keratoconus. The fit is often time-consuming and may take several different lenses to achieve the proper fit.
Piggybacking Contact Lenses – This method is used for individuals who require a gas permeable lens but cannot tolerate wearing rigid contacts. Piggybacking utilizes a soft lens placed on the eye first, and then a gas permeable lens is placed over the top. This offers the comfort of soft contacts with the rigidity and clarity of the gas permeable lenses.
Hybrid Contact Lenses – Hybrid contact lenses were designed specifically for keratoconus. This technology blends a rigid contact lens center with a softer edge, or skirt, of the contact
Scleral and Semi-Scleral lenses – These lenses are gas permeable lenses but cover a larger area of the eye than a standard rigid lens. These lenses don’t put pressure onto the cone shape of the eye. The reduced pressure results in a more comfortable fit for patients.
Prosthetic Lenses – This lens is used specifically for patients that have very advanced keratoconus and have ruled out other options. The advanced scleral lens also doubles as a protective prosthetic shell. There are special requirements to qualify for this lens though, so check with your eye care professional if this is an option for you.
Optical Coherence Tomography
Optical Coherence Tomography is a non-invasive imaging test that may be performed as a standard part of your regular, comprehensive exams, or you may be able to request this test as an addition to your usual exam.
Optical Coherence Tomography uses light waves to take cross-section images of your retina, which is the area of light-sensitive cells at the back of your eye that is responsible for receiving light and transmitting it into messages that are sent up to the brain. The technology behind OCT enables your eye doctor to see each of the different layers that make up the retina. By being able to see these and measure them, they can obtain a much clearer picture of the overall health and condition of your eyes.
Why are Optical Coherence Tomography scans important?
When you choose to have an OCT scan at fairly regular intervals, such as during your normal comprehensive eye exams, your eye doctor can compare newer results to previous ones. This helps them to build up a picture of the health of your eyes, and spot any changes which may be concerning, early, before they cause symptoms or have a permanent effect on your vision.
Anyone can have an OCT scan, but they are particularly recommended for patients over the age of 25 who are concerned about the health of their eyes, or who are at risk of or already have diabetes, glaucoma or a family history of eye disease. This is because they can be used to spot the early signs of a range of eye diseases, including glaucoma, diabetic retinopathy, macular degeneration, disorders of the optic nerve and more – even before you realize that you are affected.
What happens during an Optical Coherence Tomography scan?
An OCT scan is a quick, painless experience. To prepare you, your eye doctor may require you to have eyedrops that will dilate your pupils and make it easier to see your retina. This means that the scanner will get clearer, more concise images. You’ll be asked to sit in front of the OCT machine where you will rest your head against a support to help you sit perfectly still. As you stare ahead, the equipment will perform the scan of your eyes. There is no contact with your eyes whatsoever, you will just need to sit still, with your eyes open as much as possible during the process, which usually takes less than 10 minutes. The images will be sent digitally to your eye doctor for them to assess immediately and stored digitally on your personal record.
There’s no downtime after an OCT scan, but if you have had your eyes dilated you may find that you are particularly sensitive to light for a few hours afterwards. This occurs because the pupils remain wider and therefore able to let more light in that usual.
If you would like to find out more about Optical Coherence Tomography, don’t hesitate to speak to our professional eyecare team.
Optikam
Eye care professionals use Optikam’s technology to capture more than 3 million eyewear measurements every year. The OptikamPad iPad app is a total dispensing solution that enables eye care professionals to successfully assist patients at all stages of the eyewear dispensing process, providing them with a unique and custom patient experience.
Optikam Posture Devise (OPD)
You may be surprised to learn that wearing glasses can and likely will affect your posture. Glasses lenses are most accurate when you look directly through their center. This means if your glasses are sitting too low or have slipped down your nose, you may find that you are subconsciously tilting your head back and this can affect your overall posture.
Optikam’s OPD measurement device is a cutting-edge tool that obtains eyewear measurements that take into account how the frame will be worn by patients, enabling the fit to be customized to their individual parameters. The ten measurements taken into account when determining each patient’s position of wear include:
Monocular pupillary distance
Multifocal seg heights
Pantoscopic tilt
Rear vertex distance
Wrap (face form tilt)
Near pupillary distance
This results in frames that not only look fantastic, but that also fit perfectly, remaining both comfortable and stable on the face without you needing to adopt an unnatural posture. The measurements obtained by the Optikam OPD measurement tool are immediately visible on your eye doctor’s tablet so that they can recommend which alterations to the frames are needed to ensure that the frames fit with precision and gives you the best visual experience.
Benefits of OptikamPad and Optikam OPD
Traditionally, the process of a comprehensive eye exam, choosing frames and fitting glasses requires fairly close contact with your eye doctor or other eye care professionals. However, with social distancing being a new process variable, many patients are looking for more virtual options. Fortunately, OptikamPad makes it possible for optical stores to dispense eyeglasses with minimal human contact. This is because the OptikamPad can take measurements from a further distance or even through plexiglass screens. It can even be placed on a stand and the app operated using a Bluetooth mouse, putting even greater distance between your eye care professional and you.
If you would like to find out more about Optikam OPD and OptikamPad, our knowledgeable team would be delighted to help. Please contact us with any questions or to schedule an appointment.
Sports Vision
Sports vision is a growing niche in the eyecare industry, helping athletes improve their performance skills through the enhancement of visual skills. While regular eye exams are important for checking the health of your eyes and your visual acuity (how clearly you can see a still object at different distances), sports vision testing is recommended for anyone who takes their athletic performance seriously.
Visual skills needed for sports performance
There are several key visual skills that are enhanced through sports vision programs for athletes that aim to achieve their optimal sports performance, these include:
Dynamic visual acuity: this refers to the patient’s ability to see objects clearly while in motion. This is exceptionally important as hand-eye coordination and reflex reactions are essential for success in most sporting activities.
Contrast sensitivity: good contrast sensitivity is needed to determine the difference between an object and its surroundings. Contrast sensitivity is particularly important in situations where there may be low light, fog or glare that could diminish the natural contrast between objects and backgrounds.
Eye tracking: this refers to the ability to follow a fast-moving object, such as a ball or puck.
Switching eye focus: athletes need to be able to change their focus quickly and accurately from one distance to another.
Binocular vision skills: also known as eye teaming skills, these skills determine how well your eyes work with one another to produce a single, clear image.
Processing speed: visual processing speed is defined as the amount of time it takes to make a correct judgement about a visual stimulus – for example, how fast a ball is travelling towards them.
Peripheral awareness: athletes also need to be able to be aware of what is happening at the edges of their vision while also concentrating on a fixed object in front of them.
Sports vision testing can enable your eye doctor to spot any weaknesses that you may have in any of these key visual skills. By identifying them, it is possible for you to undergo treatment to overcome theses issues and meet your specific goals that will ultimately enhance your overall athletic performance. This is known as sports vision training.
What’s involved in sports vision training?
Sports vision training refers to a personalized treatment plan that is designed to train the brain to achieve maximum efficiency in the way that it receives, processes, and responds to visual input. Exactly what is involved in your sports vision training will depend on your athletic activity and the visual skills that your eye doctor identifies for improvement after comprehensive sports vision testing. Your treatment program will use a variety of tools, techniques, and exercises. You may also be asked to complete some exercises at home to further enhance your progress. With sports vision training, the ultimiate goal is for athletes to continue to see faster and clearer, giving them a distinct competitive edge.
For more information about sports vision and how it can benefit amateur and professional athletes, please contact our team.
Overview of Common Ocular Diseases
Both optometrists and ophthalmologists treat many common types of ocular disease. However, for the best outcome, it’s important to see an eye doctor regularly. They can identify any issues before they become serious problems.
Fortunately, they can treat all of the diseases mentioned below, and in some cases, you can do certain things to prevent them from developing. Look at the most recent statistics, and you’ll see why good eye health care matters.
Currently, more than 4.2 million people in the U.S. alone over the age of 40 are partially blind or have poor visual acuity. Although a lot of things cause these problems, the ocular diseases listed below are the most common.
Macular Degeneration
This is commonly referred to as “age-related macular degeneration” because it affects seniors. Not only does it cause blurriness and distortion but left untreated, individuals lose their central vision. In other words, they are unable to see anything through the center portion of the eye.
Two types of this ocular disease exist. First, wet macular degeneration means that abnormal blood vessels that are located behind the retina grow under the macular. Along with leaking blood and fluid, this leads to scarring and, sometimes, permanent damage. Second, dry macular degeneration progresses slowly as part of the natural aging process. Typically, it affects both eyes at some point.
Cataracts
Roughly 20 million people in the U.S. over the age of 40 have cataracts in either one or both eyes. While they can develop in children, teens, and young adults, cataracts are most often associated with age. With this, a film covers the eye, which, in turn, makes everything appear blurry.
Of all the different kinds of ocular diseases that lead to blindness worldwide, cataracts rank number two. Fortunately, an eye doctor can remove the damaged lens, followed by implanting an artificial one. After recovery, patients see amazingly well.
Diabetic Retinopathy
If you have diabetes, then you’re at risk of developing this ocular disease. This particular disease causes progressive damage to the retina’s blood vessels. The first stage consists of mild non-proliferative retinopathy and then moderate non-proliferative retinopathy, which blocks some of the vessels.
Then, it moves into stage three or severe non-proliferative retinopathy, which means more blood vessels become blocked. The fourth and final state, proliferative retinopathy, is the most advanced. Although Diabetic Retinopathy does affect just one eye on occasion, it typically involves both eyes.
Start by improving your overall health. Eat balanced meals, keep your blood pressure and cholesterol levels down, and take insulin. In addition, regular exercise, losing weight, and giving up smoking all make a huge difference. From there, a qualified eye doctor can provide you with treatment options to reduce the risk of losing your vision.
Glaucoma
Many people think glaucoma is one type of ocular disease. However, it’s a group of diseases that cause damage to the optic nerve. When that happens, people face the risk of losing their sight completely. With glaucoma, the fluid pressure inside the eyes gradually rises.
There are also two categories of glaucoma: open-angle and closed-angle. Not only is open-angle glaucoma chronic, but it also progresses slowly. Often, a person can have this type without knowing it. Unfortunately, they don’t realize there’s an issue until they have a comprehensive eye exam performed.
As for closed-angle glaucoma, it’s usually painful and it comes on suddenly. In addition, an individual can lose their vision much faster with this kind of glaucoma compared to the open-angle kind. Because this happens fast and involves pain, it’s diagnosed much quicker as well.
For these common types of ocular diseases, it’s important to have your vision checked. An eye doctor might simply diagnose you with myopia or hyperopia, followed by prescribing either eyeglasses or contact lenses. If an ocular disease is diagnosed, the optometrist will determine the best treatment plan for optimal eye health and vision.
iLux
If you have dry eye syndrome, you understand the frustration of repeatedly applying eye drops and other therapies in vain. The iLux®, a new product on the market, may help address your problem.
It treats dry eye syndrome by combining heat and pressure to clear obstructions from the meibomian glands. Learning how it works and its advantages in treating dry eyes may help you.
What Is iLux?
Millions of individuals worldwide suffer from the prevalent ailment known as dry eye syndrome. This happens when your eyes do not produce tears in sufficient amounts or when tears evaporate too soon. Discomfort, irritability, and even eyesight issues may result from this. Although several treatments for dry eyes exist, many are transient and call for repeated application.
iLux is a medical device designed to treat dry eye syndrome. It combines heat and pressure to remove blockages from the meibomian glands. These glands in the eyelids produce the oil that prevents your tears from evaporating too quickly.
The handheld device is easy to use, making it a convenient and effective solution for those who suffer from dry eyes. It is a practical choice for people with busy schedules because no downtime or recovery period is necessary.
How Does It Work?
The device works by applying gentle heat and pressure to the eyelids. This helps loosen and remove blockages from the meibomian glands. The treatment allows the glands to function properly, producing the necessary oils to keep the eyes moisturized and healthy. The device also provides targeted treatment to specific areas of the eyelids. This allows for a more customized and effective treatment experience.
Benefits
Using this medical device to treat dry eyes offers numerous benefits, including:
Improved Comfort
Dry eyes can cause discomfort, irritation, and even pain. By treating dry eyes with iLux, you can experience improved comfort and reduced symptoms.
Enhanced Vision
Dry eye syndrome can affect vision, causing blurriness or difficulty focusing. Treating the condition with iLux can help improve vision and clarity.
Noninvasive
Unlike other treatments for dry eyes, such as surgery, iLux is a noninvasive solution that requires no downtime or recovery period.
How to Use the Device
Using iLux to treat dry eyes is straightforward. Since it is handheld and portable, this device is easy to use at home and when traveling.
To use it, follow these steps:
To determine if it is a good fit for you and to get usage instructions, consult your eye doctor.
Position the device against your closed eyelid over the affected area.
It will apply gentle heat and pressure to the eyelid, helping remove blockages from the meibomian glands.
Repeat this process on each eyelid as instructed by your doctor.
After using it, you may experience some mild discomfort or redness in the treated area. These are usually not severe; they should go away within a day or two.
Conclusion
If you are experiencing dry eyes, the iLux might be the solution for you. This noninvasive medical device uses heat and pressure to remove blockages from the meibomian glands. The treatment allows for improved eye health and comfort. To learn more about the device and whether it is right, consult your eye doctor today.
Limbal Relaxing Incisions
Astigmatism is a relatively common eye disorder that causes the vision to be blurred or distorted. It occurs when the lens part of the eye, known as the cornea, isn’t perfectly curved and instead resembles a football rather than a soccer ball. This means that the light entering the eye comes through at a distorted angle, making the object appear blurry and out of focus. There are several ways in which it is possible to treat astigmatism, including laser eye surgery and corrective lenses. However, another possibility is a solution referred to as limbal relaxing incisions.
What are limbal relaxing incisions?
Limbal relaxing incisions are microscopic cuts to an area in the eye known as the limbus. This helps to relax the curve in the cornea and improve its ability to focus light correctly. It can significantly improve your astigmatism and the overall quality of your vision.
Am I a good candidate for limbal relaxing incisions?
If you have astigmatism, are over 18, in good general health and have no major eye conditions, then chances are you are a good candidate for limbal relaxing incisions. Make an appointment with your eye doctor to discuss your candidacy further.
Importance of Routine Eye Exams
Routine eye exams are an important aspect of maintaining one's overall health. As with an annual physical or dental exam, it is extremely important to have your eyes examined regularly. Regardless of how great your eyesight is, scheduling regular eye exams is a great way to stay on top of your overall health.
Adults should have an eye exam every 1-2 years, depending on any existing vision problems, eye conditions or being diagnosed with significant risk factors, such as diabetes, high blood pressure, thyroid disease, previous eye injuries or family history. The doctor will recommend a frequency for routine follow-up exams based on the patient’s medical history. For instance, a diabetic patient will need a dilated eye exam every year while contact lens wearers need exams every year in order to look for changes that might affect lens fit and eye health.
Regular eye exams will also ensure that prescriptions for glasses or contact lenses are current as well as offer an opportunity to check for early signs of certain diseases. Adults older than 60 should have an eye exam each year, as age-related eye problems are more common.
It may be important to see a doctor more frequently if one is experiencing any of the following:
Blurry vision or loss of vision.
Difficulty seeing things near and/or far away and perform basic tasks.
Flashing light in the eye.
Eye floaters, or small spots that appear in vision.
Why Should You Have Regular Eye Exams?
While eye exams are important for one's vision, routine eye exams can also help to identify a variety of problems ranging from cognitive decline to diabetes. Since the eye is an extension of the brain and the only part of the body where blood vessels and tissue are visible, it allows an eye doctor to detect warning signs of the early stages of different health problems, such as diabetes which can present as bleeding in the eye or swelling in parts of the retina.
Besides diabetes, there are several other health problems that may be detected during a routine eye exam such as brain tumors that may cause swelling of the optic nerve and rheumatoid arthritis or other autoimmune disorders which may be the reason behind dry eyes.
Skin cancer on the eyelid is another health risk as the eyelid is very sensitive to ultraviolet rays and may be one of the first places affected by different types of skin cancers. Any spots or affected areas may be detected before skin cancer can spread to other parts of the body.
Addition, high blood pressure which would show as blood vessels in the back of the eye appearing bent or leaking, the narrowing of the vessels in the retina, swelling of the optic nerve, and hypertensive retinopathy in its earliest stages can be looked for during the exam.
There are also some progressive eye diseases that are not immediately apparent and should be tested for during regular eye examinations including:
Glaucoma which is the buildup of pressure within the eye that causes damage to the optic nerve and can lead to a loss of peripheral vision or a complete loss of vision. Glaucoma is a chronic, progressive eye disease that doesn't show any symptoms or pain in the initial stages.
Macular degeneration is an eye condition that causes damage to the retina.
Cataracts which is the most common cause of blindness in the world. Cataracts occur when the lens of the eye becomes less flexible with age. Blurred or foggy vision and sensitivity to light are common symptoms. Cataracts are easily corrected with outpatient surgery.
Vision changes can have a profound effect on a person’s day-to-day life, but early treatments can help to slow or stop vision loss and regular eye exams can help ensure a lifetime of clear sight
OCuSOFT
Clean eyes are healthy eyes. Nevertheless, our eyes are exposed to countless potentially harmful microorganisms during the course of an ordinary day. This could be anything from dust and pollen, which could cause allergies, or infection-causing bacteria. Daily cleansing is the best way to keep eyes clean and free from debris, but to maximize the effects of your cleaning, it’s important to use products that are designed just for your eyes. Thankfully, there is OCuSOFT.
A large part of the OCuSOFT product line is a selection of non-irritating products that are designed specifically to help remove any oil, debris and pollen from the eyelids and eyes, leaving them as clean and healthy as possible. Here are some of the products that you may be interested in:
OCuSOFT Lid Scrub
One of the most popular product categories in the OCuSOFT line, this lid scrub takes the form of a foaming eyelid cleaner. The instant foaming formula helps to remove oil, debris, pollen and contaminants and should be used with a new, soft, clean cleansing pad for each eye. Choose the Platinum Foam variety for extra-strength and additional anti-inflammatory properties that helps to soothe eyes and remove irritation as soon as it is applied.
OCuSOFT Lid Scrub Pre-Moistened Pads
These extra-strength pads are a leave-on formula. Simply place them onto your eyes and relax. While you do so, the formula cleanses your eyelids and removes any contaminants to provide relief from irritation. This product is recommended for moderate to severe eyelid conditions.
OCuSOFT HypoChlor
This product is available as both a gel and a spray and should be used in combination with a surfactant such as OCuSOFT’s lid scrub for the greatest possible level of cleanliness.
OCuSOFT Dry Eye mask
As the name of this product suggests, this mask is designed to help combat a condition called dry eye. Dry eye occurs when the eyes don’t make enough tear film, the quality of the tera film is compromised or it drains away too quickly. The OCuSOFT dry eye mask is a moist heat mask that contains a patent-pending cross hatch design proven to deliver even heat distribution across the eyes. This warmth helps to break up any hardened oil deposits in the meibomian glands that may be contributing towards dry eye.
For more information on keeping your eyes clean and healthy, or to find out more about OCuSOFT products, please speak to our dedicated and professional eyecare experts.
LASIK Procedure
If you are one of the thousands of people considering LASIK laser eye surgery, then you will probably be gathering as much information as possible about the treatment. By this point, you are probably aware of the benefits that LASIK offers, such as a reduced or eliminated need for glasses or contact lenses and greater convenience in your day to day life. However, for many patients, despite the advantages of LASIK, the thought of surgery on their eyes is still a cause of anxiety and fear. One of the best ways to alleviate this concern is to find out more about what the procedure entails.
Your consultation
Before you can be approved for any form of laser vision correction, including LASIK, you will need to attend a consultation appointment with your surgeon. During the consultation, he will perform an examination of your eyes and use your medical and ocular history to determine if you are a good candidate for the procedure. He will also speak to you about the expected outcome from your surgery, making you aware that while LASIK will dramatically improve your eyesight, there is no guarantee that you will not need to wear glasses in some situations, such as while driving in the dark.
How LASIK Works
LASIK uses a cool, ultraviolet beam of light to reshape the patient’s cornea. Doing so will more accurately focus the light that enters the eye on to the retina, thus improving the patient’s vision. The way in which the cornea needs to be reshaped will depend on the visual needs of the patient. For example, a patient who is far-sighted will need their cornea reshaping to be steeper to experience better eyesight. Alternatively, a patient who is near-sighted will require their cornea to be flattened in order to improve their vision. LASIK can also smooth an irregular cornea into a more standard shape, meaning that the procedure can also be used to correct astigmatism.
The LASIK procedure
The LASIK procedure is very fast and straightforward. Although you will probably be in the surgical suite for around half an hour, the actual process only takes a couple of minutes per eye. The rest of the time will be spent preparing and ensuring that you are comfortable. Anesthetic eye drops are given to patients before their procedure so that the entire process is pain-free. If you are particularly anxious, it may also be possible for you to be slightly sedated – this should be discussed with your doctor at your consultation appointment.
Once you are in position, we will use a femtosecond laser to cut a thin, circular flap into the outer cornea. This can then be pulled back to reveal the underlying corneal tissue, known as the stroma so that it can be reshaped using the laser. The exact path that the laser needs to take, known as the topography, will have been pre-programmed ahead of the procedure and can be followed with complete precision and accuracy.
Once the reshaping is complete, the flap is replaced back over the eye and the surgery is complete. There is no need for sutures or bandages as the cornea will start to heal immediately and without any medical intervention.
Eye Disease Treatment
Millions of patients are diagnosed with diseases and conditions of the eye every year. Some of which may not display symptoms until there is irreversible damage to the patient’s vision. The outcome of eye disease can range from temporary discomfort to total loss of vision, which is why all eye problems and diseases should be taken seriously and regular eye check-ups are absolutely essential.
What Are The Causes of Eye Disease?
The main causes of eye problems can be divided into five groups:
Inflammation of the eye and surrounding structures caused by a bacterial, viral, parasitic or fungal infection.
Injuries to the eye and surrounding structures, either as a result of trauma or an object in the eye.
Genetically inherited eye diseases, many of which may only manifest later in life and affect the structures and the functioning of the eye which therefore can impair visual abilities. In some cases, however, children are born with these conditions.
Diseases or conditions, such as migraine or diabetes, which can affect other organs of the body, such as the eyes.
External causes, such as allergies or eye strain due to over-use, or as a side effect of medication.
What Are The Symptoms of Eye Disease?
The three symptoms indicative of eye disease are changes in vision, changes in the appearance of the eye, or an abnormal sensation or pain in the eye.
Changes in vision can include the following symptoms:
Nearsightedness is caused by an elongation of the eyeball over time, making it difficult to clearly see objects far away.
Farsightedness is caused by the shortening of the eyeball, making it difficult to see objects that are close-by clearly.
Blurry or hazy vision, or loss of specific areas of vision, which can affect one or both eyes and is the most common vision symptom. Any sudden changes in vision should be a cause of concern.
Double vision means a single clear image appears to repeat itself. This could be accompanied by other symptoms like headaches, nausea, a droopy eyelid, and misalignment of the eyes.
Floaters are specks or strands that seem to float across the field of vision. These are shadows cast by cells inside the clear fluid that fills the eye. These are usually harmless, but should be checked out as they could point to something serious such as retinal detachment.
Corneal Refractive Therapy
Corneal refractive therapy, also known as CRT, is a simple, painless treatment for refractive eye errors like myopia and has two core benefits. First, it can be used to help patients see clearly during the day without using glasses or contact lenses, giving them the freedom and flexibility that they need to live life to the fullest. Second, CRT has been shown to help slow the progression of myopia, keeping prescriptions under control and potentially reducing the likelihood of patients developing serious eye health problems associated with high myopia in the future.
Here’s everything that you need to know about corneal refractive therapy and what it means for you.
Understanding refractive eye problems
Refractive eye problems like nearsightedness, farsightedness and astigmatism are extremely common, with nearsightedness – also known as myopia – being the most common of all. Patients with myopia can see nearby objects clearly, but those further away become progressively more blurred. Refractive eye errors occur when the shape of the clear dome covering the front part of the eye, called the cornea, impair the light-bending and focusing process in your eyes. This leads to the light ending up in the wrong place inside the eye, and the message that is sent to our brain from our eyes is muddled, causing blurred vision.
What is corneal refractive therapy?
Corneal refractive therapy was initially developed as a treatment to correct and slow the progression of nearsightedness. However, it has also been found to be effective at controlling other refractive errors, including farsightedness, astigmatism and an age-related refractive condition called presbyopia.
CRT is a non-invasive, painless and straightforward method of correcting patient vision so that they don’t need to wear contacts or glasses, and they don’t need laser vision correction surgery to see clearly. CRT uses special contact lenses that are worn overnight and apply light pressure to the cornea in order to reshape it so that light is refracted correctly, and the image sent from the eyes to the brain is clear. The cornea is able to retain this new shape even after the contact lenses are removed the next morning, meaning that you can continue to see clearly for several hours. The more consistently you wear your CRT lenses overnight, the longer your eyes will learn to retain their new shape and eventually, patients can enjoy up to 48 hours of clear vision without using prescription lenses. However, the effects aren’t permanent so if you stop wearing the lenses, your vision will gradually return back to normal over the course of a few days.
Slowing the progression of myopia with corneal refractive therapy
Another key benefit of CRT is that it can actually help to slow the progression of myopia. Most people who are nearsighted find that their eyesight gets progressively worse as they get older. This deterioration may not be rapid, but it can end in patients requiring high prescriptions. Studies have found that patients who have high myopia are more likely to develop serious eye problems in the future, including glaucoma, macular degeneration, cataracts and a detached retina. Regular use of your corneal refractive therapy lenses could help keep your prescription stable and lower your risk of developing these problems.
Am I a candidate for corneal refractive therapy?
You may be a candidate for corneal refractive therapy if you:
Have a myopia prescription within specific parameters
Have a prescription for hyperopia, presbyopia or astigmatism within specific parameters
Have stable vision, which means that your prescription hasn’t changed during the last two years
Are not a suitable candidate for laser vision correction
Have a job that makes it impractical or unsafe to wear glasses or contact lenses
Enjoy hobbies that make it impractical or unsafe to wear glasses or contact lenses
Have healthy eyes and are generally in good health
For more information, please contact our friendly and knowledgeable team today.
Neurolens
Neurolens are the first and only prescription lenses that include an element of contoured prism in their design. This prism is designed to bring the patient’s eyes into more equal alignment, and this should help to provide relief from the symptoms that are associated with several eye misalignment conditions, including digital eye strain and binocular vision dysfunction.
What is digital eye strain?
Digital eye strain is the name given to describe a group of symptoms that can occur when someone spends long periods of time using digital devices. Since using digital devices requires the eyes to work harder than normal and we don’t always position our devices the perfect distance away, it can lead to issues such as eye pain, dry and irritated eyes, eye fatigue, light sensitivity and blurred vision. Unsurprisingly, the number of people who are experiencing digital eye strain has grown significantly over the last few years and is expected to continue to do so.
What is binocular vision dysfunction?
Binocular vision dysfunction, also known as BVD for short, is another eye condition but is one that is very misunderstood. Binocular vision dysfunction occurs when the eyes aren’t perfectly aligned, causing your brain and eyes to work harder than normal in order to create a clear visual image and remain focused. This places pressure on the trigeminal nerve, which is the nerve that is responsible for the majority of the sensations that we experience in our head and back. BVD can often manifest as other things owing to the huge range of symptoms that are associated with the condition. These can include, but aren’t limited to:
Blurred vision
Headaches/migraines
Double vision
Motion sickness
Vertigo
Dizziness
Anxiety
Many people don’t think to visit an eye doctor when they are experiencing these symptoms, but all can occur simply because the eyes are out of alignment.
What are Neurolens lenses and how do they help?
As well as containing your usual prescription, Neurolens lenses also contain a specific amount of contoured micro-prism. This micro-prism alters the position of images so that they are aligned in the same plane. This then reduces the pressure on the muscles around the eyes as well as bringing the eyes into alignment, easing the symptoms that the patient has been experiencing.
The amount of prism in Neurolens lenses is decided using the Neurolens eye-tracking device. This non-invasively measures the misalignment that the patient is experiencing, and this is used to form the basis for the patient’s Neurolens prescription. After this, it’s fairly normal for the amount of prism to need to be adjusted by infinitesimal amounts to achieve the optimal relief from your symptoms. Most patients who choose Neurolens treatment see a 50% improvement in their vision as soon as they start to have micro-prism incorporated into their prescription lenses. However, with careful adjustments, many patients see as much as an 80% reduction in the effects of digital eye strain and binocular vision dysfunction.
Want more information about Neurolens? Please contact our knowledgeable eye care specialists.
MacuHealth
There are many different elements that make up our eyes. One of these is the macula. This is part of the retina, which is found at the back of the eye. The macula contains a high concentration of light-sensitive cells. As they detect light that passes through the eyes, these cells send signals to the brain which then interprets them as images.
The macula contains three pigments. These are: lutein, zeaxanthin and meso-zeaxanthin. To preserve the health of the macula it’s necessary to maintain a deep layer of macular pigment. This will help to protect the cone cells from oxidative stress, keeping them healthy and functioning optimally for longer. The best way to achieve this is to find ways to replenish the macular pigment so that it remains thick and offers the greatest protection from the type of damage that characterizes eye diseases such as macular degeneration.
It’s true that lutein and zeaxanthin can be found in certain foods such as dark, leafy vegetables and citrus fruits, but you would need to consume large amounts to give the level of these nutrients an effective boost. Meanwhile, meso-zeaxanthin is much harder to increase through consumption alone. Fortunately, there is another option – supplements. Studies have shown that taking supplements that contain all three macular pigments can slow the progression of conditions like macular degeneration and keep vision optimized for longer.
Macular Degeneration
Macular degeneration, commonly referred to as age-related macular degeneration (AMD), is the single largest cause of sight loss in the developed world and affects more than 10 million Americans. It usually affects people over the age of 60, but has been known to affect those who are younger. It is a painless condition that usually affects both eyes with the loss being experienced in the central vision. It does not affect the peripheral vision, meaning that it does not cause total blindness.
What is the macula?
The macula is the most sensitive part of the retina and is responsible for our central vision and what allows us to see fine details with clarity.
Varieties of AMD
Wet AMD
Wet AMD is one variety of the condition in which abnormal blood vessels grow into the macula, leaking blood or fluid which then causes scarring and a rapid loss of central vision. Wet AMD can develop suddenly and rapid referral to a specialist is essential as it can be treated if caught quickly.
Dry AMD
Dry AMD is the most common variety of age-related macular degeneration and is a gradual deterioration of the retina as the cells die off over time and are not regenerated. Up to 15% of people with dry AMD go on to develop wet AMD, and so any sudden changes in your vision should be followed up with your optometrist as soon as possible.
Latisse Eyedrops
Many people don’t realize that eyelashes are both functional and attractive. The purpose of eyelashes is to act as a first line of defense for our eyes, preventing airborne dirt, dust and other debris from reaching the delicate tissues of our eyes. You probably don’t know that when your eyes are closed, your eyelashes form a nearly impenetrable barrier against foreign irritants entering the eyes.
Unfortunately, we aren’t all blessed with naturally thick, luscious lashes. In fact, many people choose to get artificial eyelashes or eyelash extensions to make them appear longer or thicker than they really are. Unfortunately, the challenge of achieving voluminous eyelashes is even greater if you suffer from a condition called hypotrichosis.
Dry Eye Treatment
Dry Eye can have a major impact on your quality of life. You may find your eyes get tired faster or you have difficulty reading. Not to mention the discomfort of a burning sensation or blurry vision. Let’s take a look at dry eye treatments – from simple self-care to innovative prescriptions and therapies – to help you see clearly and comfortably.
What is Dry Eye?
Understanding dry eye will help you determine the best treatment option. Dry eye occurs when a person doesn't have enough quality tears to lubricate and nourish the eye. Tears reduce eye infections, wash away foreign matter, and keep the eye’s surface smooth and clear. People with dry eyes either do not produce enough tears or their tears are poor quality. It’s a common and often chronic problem, especially in older adults.
Preventive Self-Care
Before we delve into more serious dry eye treatment options, here are a few simple self-care options that can manage minor cases of dry eye.
Blink regularly when reading or staring at a computer screen for a long time.
Make sure there’s adequate humidity in the air at work and at home.
Wear sunglasses outside to reduce sun and wind exposure. Wraparound glasses are best.
Take supplements with essential fatty acids as these may decrease dry eye symptoms.
Drink 8 to 10 glasses of water each day to avoid dehydration.
Find out if any of your prescriptions have dry eye as a side effect and if so, see if you can take an alternative.
Artificial Tears
For mild cases of dry eyes, the best option is over-the-counter eye drops. Here are a few tips for selecting the right one:
Low viscosity – These artificial tears are watery. They often provide quick relief with little or no blurring of your vision, but their effect can be brief, and sometimes you must use these drops frequently to get adequate relief.
High viscosity – These are more gel-like and provide longer-lasting lubrication. However, these drops can cause significant blurring of your vision for several minutes. For this reason, high-viscosity artificial tears are recommended at bedtime.
Prescription Dry Eye Treatments
There are several prescriptions that treat dry eye differently. Your eye doctor can advise the best option for your situation.
Contact Lenses – There are specialty contact lenses that deliver moisture to the surface of the eye. They’re called scleral lenses or bandage lenses.
Antibiotics– If your eyelids are inflamed, this can prevent oil glands from secreting oil into your tears. Your doctor may recommend antibiotics to reduce inflammation.
Understanding PRK
Understanding PRK: Is It Right for You?
PRK or photoreactive kerectomy is a surgical procedure that was the precursor for the surgery known as Lasik. The biggest difference between the two procedures is how the first portion of the operation is conducted. Additional variability between the two procedures includes recovery, risk factors, and the patient’s overall needs. Understanding these differences can help you decide if PRK is an appropriate solution for your vision issues.
How it Works
PRK utilizes a laser to correct farsightedness (hyperopia), nearsightedness (myopia), and astigmatism. During a PRK operation, a laser is used to remove the exterior epithelial cells from the cornea. This procedure uses an excimer laser to remove the cells which are then discarded. A contact “bandage” is placed over the eye, and the cells can heal over the course of a few days. Your doctor will then remove the contact lens when the eye has healed enough to be exposed.
While the results are like that of Lasik, PRK does take some additional healing time. This is due to the time that must be allowed for the epithelial cells to heal and regrow on the eye. Additionally, Lasik patients generally experience less discomfort and faster results. PRK results can take a few weeks to fully materialize.
This isn’t to say that PRK doesn’t have its own benefits too. This procedure is well-suited for patients that have had previous eye surgeries and may have thin corneas. Because PRK does not make an incision into the cornea and only removes the epithelial cells, it leaves more of the stromal tissues which underly the epithelial tissue. PRK does not run the risk of “flap” issues that can arise from Lasik, and the risk of removing too much of the cornea is reduced. However, if you are considering PRK, you should consult with your medical professional to identify the right procedure for your specific case.
Before the Surgery
When you meet with your eye specialist to discuss your options, there are several factors that they will consider. Your potential surgeon should conduct a thorough eye exam during which they will measure your eye moistness, pupil size, corneal thickness, and corneal curvature. Your doctor should also review your medical and family history to identify any possible concerns about your suitability. Make sure that you bring a list of your medications and previous operations. Finally, you may be required to stop wearing contact lenses for a period before the operation. This can allow your cornea to return to its natural shape before the operation.
The Surgery
The actual PRK surgery is a short procedure that will only take about 15 minutes. The patient will not be sedated during the operation but may be given an oral sedative that helps to relax the eye. Numbing drops are applied to your eyes and a small speculum is also used to hold the eyelids open for the procedure. The excimer laser is programmed for your exact eye prescription. Patients are instructed to look at a certain object or target while the laser is operating. The surgeon will watch the procedure through a microscope and can stop the procedure at any time. Most patients do not report discomfort, although there may be some pressure.
Recovery
You will be observed for a short time after your operation to make sure that you don’t have any severe immediate reactions. After this observation, you will be sent home. It is important to have someone else drive you after any procedure that may impact your vision or ability to drive safely. You should make sure to follow all of the doctor’s recommendations to facilitate a speedy recovery. You should also expect several follow up appointments to make sure that the operation was successful and that there are no additional concerns.
Your full results may take several weeks, but almost all patients have vision that is 20/40 or better. Over time, as the eye ages, vision may naturally degrade. At this time, you should consult with your medical professional to see if an additional operation is a good option for you.
Can Diet Reverse Diabetic Retinopathy
Eye disease that is caused by diabetes is currently the number one cause of blindness and vision loss. Due to the increased risk in diabetic patients, doctors recommend that people over 30 with diabetes get an annual dilated eye exam. Diabetic patients under 30 should get this exam five years after they have been diagnosed.
Diabetic retinopathy is a condition that is caused by damage to the retina. Patients that have diabetes may also have experienced extended periods of time where their blood sugar was elevated. The high levels of blood sugar damage the retina’s walls which leave them susceptible to leaking. When fluid accumulates in the retina or macula, it causes vision loss.
To make these matters worse, if prolonged high blood sugar levels are seen again, the retina will be oxygen-depleted. This causes the abnormal growth of new blood vessels. This condition is called neovascularization. This blood vessel type is weak and prone to leaking. As these blood vessels leak, they introduce blood into the eye. Excessive bleeding into the eye can cause blindness.
Treatment
While a healthy diet and exercise can be beneficial to your optical health, diabetic retinopathy is a condition that is caused by damage to the retinal wall. While this damage can sometimes be corrected, simple diet changes won’t reverse the effects.
It is essential to catch the condition in the earlier stages to reduce the effects. This can also help patients understand the importance of monitoring their blood sugar so that repeat events can be limited. Treatment options are even more successful when diabetic retinopathy is caught early. These options include vitrectomy, scatter photocoagulation and focal photocoagulation.
During both scatter, and focal photocoagulation the doctor will use lasers to help alleviate the condition. The lasers make small burns on the retina aimed at the blood vessels. These burns will help to seal the blood vessels to prevent more leakage and stop them from growing larger.
When using scatter photocoagulation, hundreds of small burns are made in a specific pattern during two additional appointments. Scatter coagulation should be used on patients who do not have advanced diabetic retinopathy.
Focal photocoagulation specifically targets the leaking blood vessels that are in the macula. Unfortunately, this procedure is not aimed to correct the blurry vision associated with diabetic retinopathy, but it does stop it from progressing further. Once the retina has detached, neither form of photocoagulation can be used.
Vitrectomy is a surgery that helps to remove scar tissue and/or the fluid that is clouded with blood that has been leaked into the eye. This operation is the most successful when performed before the disease has progressed too far. When the operation only targets removing the fluid, success rates are very high for the procedure. When the procedure also aims to reattach the retina, the failure rate is around 50%.
EnChroma Lens Technology
If you find it difficult to tell colors apart, you may be color blind. Color blindness, or color deficiency, is estimated to affect around 8% of men and about 1% of women, but for those affected, it can significantly impact the quality of their day-to-day life. Contrary to popular belief, being color blind doesn’t mean that you can’t see any color at all. Instead, patients simply struggle to differentiate between certain colors. The vast majority of people who are color blind find it impossible to tell the difference between varying shades of red and green. You may hear this referred to as red-green color deficiency. However, this doesn’t only mean that they mix up red and green. They can also mix up colors that have some green or red light as part of their whole colors, for example purple and blue. This is because they are unable to see the red light that forms part of the color purple.
As you can probably imagine, this type of visual impairment can be a problem for things like traffic lights, taking medications and even looking at signs and directions. For example, someone who is color blind may find that the green on a traffic light may appear white or even blue.
EnChroma lens technology is specifically designed to counteract red-green color deficiency and enable patients to better identify the difference in these colors or shades. They do this by selectively filtering out the red and green wavelengths of light at the exact point where the color sensitivities overlap before hitting the retina, creating far greater contrast between the colors so that the patient can distinguish between them successfully. Most cases of color blindness respond well to EnChroma’s innovative spectral lens technology, giving patients the ability to experience life in bright, vibrant technicolor.
EnChroma lenses are made from leading edge, Trivex material, and this helps to give them the best possible quality and clarity of vision. These lenses are also extremely light, strong and offer patients 100% protection against UV light, helping to keep your eyes healthy as well as improving your vision.
If you or someone you know is color blind or color deficient and could benefit from EnChroma lenses, contact us today to learn more about how they can help!
Optomap
Optomap is an innovative new technology that gives eye doctors the ability to perform ultra-wide retinal imaging that is far superior to what can currently be achieved using conventional retinal imaging options. In contrast to conventional retinal imaging, Optomap captures at least 50% more of the retina in a single capture, and with Optomap’s multi-capture function, up to 97% of the retina can be viewed. This gives eye care professionals greater opportunity to monitor the health and condition of patient vision.
Why is Optomap important?
Optomap is another great preventative eyecare technology tool. By allowing your eye doctor to have a comprehensive view of your retina, they will be able to detect any developing eye diseases early on, before they have a detrimental impact on your vision and day to day life. Not only can Optomap detect eye conditions such as retinal holes, retinal detachment, macular degeneration and diabetic retinopathy, but it can also be used to identify some general health conditions such as cardiovascular disease, stroke and cancer.
What to expect from Optomap scanning
Optomap is a fast, painless and non-invasive procedure that is suitable for patients of all ages, even children and pregnant women. Many patients require their eyes to be dilated ahead of the scan and will be given eyedrops which will widen their pupils and make it easier for the camera to see the structures inside the eye. Pupil dilation is painless, but patients may feel more sensitive to light both during their Optomap scan and afterwards for up to 24 hours. You may also have slightly blurred vision for a few hours. Once your eyes are dilated, you’ll be sat down and asked to look into a small device that will take the pictures of your retina. A short flash of light will let you know that the image has been taken, and the entire imaging is over in just a few seconds. The results will be sent digitally to your eye doctor who will then evaluate them. The results will also be stored on your personal optical record for future information.
If you would like more information about what is involved in Optomap, or to schedule an appointment for this effective screening technology, please contact our eyecare team.
Best Foods for Eye Health
Generally, despite knowing how important the role of our eyes is in our day to day functioning, we tend to neglect the day to day care necessary to maintain optimal eye health. Just close your eyes for a minute or you put a non-transparent cloth across your eyes and try to walk around your home or workspace. It is quite difficult, right? That is how indispensable the eyes are.
While it is common knowledge that eye issues are a result of eyestrain or aging, most people are ignorant of the fact that an unbalanced diet, as well as deficiency in certain nutrients, can also facilitate eye issues. This implies that eating healthy means that there are certain nutrients that can help reduce the risk of eye issues. Some of these nutrients include omega-3 fatty acids, lutein, copper, zeaxanthin, zinc, vitamin E, A, C, and beta-carotene. For healthy eyes, there are foods that should be part of your diet daily. They include:
1. Fish- Fish is very rich in omega-3 fatty acids, especially oily fish which have oil inside their body tissue and guts. They are regarded as the major source of omega-3 fatty acids which help in improving the immune system and brain function. More so, it helps in the development of the eye and retina and in keeping the eyes from dryness. It is therefore important to incorporate fish into your diet about 3 times a week. Incorporating fish rich with this needed nutrient such as salmon, tuna, sardines, trout, herring, mackerel, and anchovies about 3 times a week is important in helping to maintain optimal eye health.
2. Eggs- The yolk of an egg contains a combination of the nutrients vitamin A, zeaxanthin, and lutein which help to safeguard the cornea, reducing the chances of suffering from cataracts and macular degeneration and zinc which keeps the retina healthy and aids night vision. Eggs are very complimentary food as it can go with other foods and can also take various forms based on your taste.
3. Carrots- This is the most common food for eye health. It contains beta-carotene and vitamin A which protect the surface of the eyes and help to prevent infections. Vitamin A is a form of protein known as rhodopsin and it is tasked with the responsibility of aiding the eyes in absorbing light. A lack of vitamin A is the reason why there are about 500 thousand blind children every year. Carrots are easy to get and very affordable. They can serve as snacks or be sliced or diced into salads.
4. Nuts and Legumes- Legumes and nuts provide a lot of vitamin E and omega-3 fatty acids which guard the eyes against age-related disorders. Brazilian nuts, peanuts, walnuts, lentils, and cashews are perfect examples of legumes and nuts and can be eaten as a form of dessert or taken as snacks based on your choice.
5. Citrus Fruits- Citrus fruits are rich in vitamin C, an essential nutrient for healthy eyes. Vitamin C helps in keeping the blood vessels in the eyes healthy. It also stands against cataracts, and with other nutrients, it helps against macular degeneration. Citrus fruits include oranges, grapefruits, and lemons. The good thing about this food is that they can be consumed on their own or turned into a juice.
Cataracts
If you’ve been diagnosed with cataracts, you may wonder if cataract surgery is right around the corner. Not to worry. There are many preventive steps you can take to slow the progression of cataracts and preserve your vision. That doesn’t mean you won’t eventually need surgery, but you can at least delay the need for quite a while.
Protect Your Eyes from the Sun
The National Eye Institute recommends protecting your eyes from the sun's harmful ultraviolet (UV) and high-energy visible (HEV) rays by always wearing good quality sunglasses while outdoors. Look for sunglasses that block 100 percent of UV rays and absorb most HEV rays with large lenses or a close-fitting wraparound style. Remember that the peak hours for sun exposure are between 10 am and 3 pm or 11 am and 4 pm during daylight savings time and that the sun’s rays are strong enough to pass through clouds, so you need your sunglasses every day.
Avoid Steroid Eye Drops
Steroid eye drops are routinely prescribed to treat dry eyes or an arthritic flare-up in the eyes. Unfortunately, they can also speed up the progression of cataracts. Talk to your Optometrist about how you can manage both conditions without inadvertently making your cataracts worse – and hastening the need for surgery.
Check Your Medications
There are over 300 commonly prescribed medications with side effects that may impact cataract progression. Since your primary care physician may not have access to your eye doctor’s medical records, be sure to ask your doctor if your current medications will affect your cataracts. If you must stay on the medication, it’s even more important to avoid sunlight during peak hours and to wear sunglasses.
Specialty Contact Lenses
Every patient is different and so are their eyes. This means that there need to be different types of contact lenses to suit each individual. Some patients have corneal abnormalities which mean that conventional lenses won’t sit comfortably on the surface of their eyes, while others suffer from eye conditions that mean normal contact lenses won’t be comfortable or could irritate their eyes.
As you may have guessed from the name, specialty contact lenses are unconventional contacts that are designed for patients that regular contacts might not be suitable. Here are some of the main types of speciality contact lenses and who they are recommended for.
Who might be a good patient for specialty contact lenses?
Some of the patients that might benefit from specialty contact lenses include those who:
have been diagnosed with dry eye syndrome
have corneal scarring
have been diagnosed with keratoconus, a condition characterized by the bulging of the cornea
suffer from strabismus, a condition where the patient has an eye that turns in or out relative to the other
have suffered an injury to the eye
suffer from a peripheral corneal thinning disorder
are intolerant to other types of lenses
Your eye doctor or contact lens provider will be able to tell you if you need specialty contact lenses and if so, which lenses would be best based on your individual requirements.
Rigid Gas-Permeable Lenses
Also known as RGP lenses, these are made from a special material that allows oxygen to pass through them and reach the surface of the eyes. This helps to keep the eyes hydrated and comfortable, making these lenses easier to wear, especially for patients who suffer from dry eyes. Dry eyes aren’t just a symptom, but a very real condition, characterized by dry, stiff, and uncomfortable eyes, blurred vision, and eye fatigue. RGP lenses are more rigid than soft lenses, and this helps to keep them stable and secure on the eyes so that patients can enjoy sharper vision. They also help the cornea to maintain its shape, which helps to minimize the effects of some corneal abnormalities.
Scleral Contact Lenses
Scleral contact lenses are very different to standard contact lenses. This is because scleral lenses are much larger in diameter, with three different sizes available depending on your specific needs. This size difference means that the edges of the contact lens fall on a white part of the eye, called the sclera rather than the cornea. Scleral lenses are also different in that they vault over the surface of the cornea rather than touching it, leaving a space between the front surface of the eye and the back of the contact lens. This makes scleral lenses a good choice for patients with dry eyes and corneal abnormalities. Space can trap tear film which keeps the eyes hydrated, while space also accommodates many corneal abnormalities, such as the bulge associated with keratoconus.
Limbal Fit Contact Lenses
Limbal contact lenses are another type of specialty lens that falls between rigid gas-permeable lenses and scleral varieties in terms of their size. Their larger overall diameter helps to increase their stability on the surface of your eyes. They also offer minimal interference with the eyelids, which helps to ensure comfort and clarity of your vision.
Hybrid Contact Lenses
Hybrid contact lenses are a combination of both soft and gas-permeable contact lenses, giving patients the opportunity to enjoy the best parts of both designs. The middle part of hybrid lenses is made from gas-permeable material that lets oxygen pass through to the eyes. However, the gas-permeable part of the lens is more rigid, and this firmer center gives the lens greater stability and the patient enhanced clarity. The RGP portion of the lens also helps to trap a tear film between the cornea and the lens so that the eye remains hydrated. Meanwhile, the outer edge of hybrid lenses is a soft lens skirt. This means that patients don’t have to deal with the hard edges associated with RGP lenses that may be uncomfortable. Instead, the comfort levels that patients experience are more like wearing fully soft lenses.
For more information about specialty contact lenses, don’t hesitate to speak to our dedicated eye care team.
Implantable Contact Lenses
If you dislike wearing glasses and you are not a suitable candidate for laser eye surgery, then implantable contact lenses (ICL’s) may offer the permanent vision correction solution that you require.
How do implantable contact lenses work?
Implantable contact lenses basically work in exactly the same way as standard, external contact lenses do. ICL’s alter the shape of the cornea in order to correct refractive errors such as near and far-sightedness, and astigmatism. However, unlike non-permanent contact lenses, ICL’s are surgically placed inside the eye rather than over the top of it.
Implantable contact lenses are also sometimes known as phakic intraocular lenses (IOL’s). The reason for this is because the two share a number of characteristics. IOL’s are seen in cataract surgery where they take the place of the affected natural lens after it has been removed. However, when used as implantable contact lenses they work in conjunction with the natural lens of the eye in order to correct your vision.
What happens during the procedure?
The procedure requires your surgeon to make a tiny incision into the cornea to allow access to the natural lens underneath. The ICL is then inserted through the incision and placed either in front of or behind the iris which is the colored part of your eye and in front of the natural lens. The incision into the cornea is able to heal naturally without stitches, and the entire process is extremely quick.
Will it hurt?
Your surgeon will give you anesthetic, usually in the form of eye drops, ahead of the procedure and therefore you should experience very little, if any, discomfort.
Which Patients are Good Candidates for Premium IOL
Premium IOLs or intraocular lenses are lenses that are placed in the eye during cataract surgery. The lens placement is designed to restore the natural lens shape. These lenses can also be placed as a vision correction device called refractive lens exchange. Premium IOLs offer advanced features beyond the single vision IOL’s that are also offered. These features include aspheric, toric, accommodating, and multifocal IOL’s.
Understanding Premium IOL Types
Aspheric Lenses
These lenses closely match the natural curve of the eye. Typical lenses were uniformly curved making it easier to manufacture, but at the same time increasing the chance of causing imperfections in vision. Aspheric lenses help to reduce imperfections and improve clarity, especially at nighttime.
Toric IOLs
These lenses are specifically designed to help correct nearsightedness, farsightedness, and astigmatism.
Accommodating IOLs
Accommodating IOL’s can tilt slightly forward when you look at objects that are close to the eye. This helps to improve visibility when you are performing actions like reading a book. While they are not necessarily as sharp as bifocals, patients have a reduced need to use reading glasses while still maintaining excellent distance vision.
Multifocal IOLs
If you require a bifocal or trifocal lens in your glasses, this may be a likely choice for you. Different portions of the lens allow for better vision at different ranges. However, there are some overall sacrifices with vision clarity at a distance.
History of Premium IOLs
Premium IOLs have been approved by the Food and Drug Administration (FDA) since the 1980s. Prior to FDA approval, when patients had cataract surgery, they were required to wear very thick eyeglasses or specialized contact lenses to correct their vision. New technologies in the optical world have allowed for a wide variety of available premium IOLs and figuring out which specific type that suits you best will depend on some different factors.
Patient Factors
Physicians are careful to discuss the realities of this procedure with their patients. After recovering from cataract surgery, many patients expect that their vision will be completely restored to their peak performance. However, doctors are careful to warn against this and explain the realities of the surgery and as well as likely expectations of what will result from the surgery. For this reason, surgeons are likely to have some initial concern about the desired outcome for the patient to make sure that their hopes are grounded.
Surgeons will also have an eye toward the patient's desire to not wear eyeglasses. If the patient does not mind wearing corrective lenses without the need for surgery, this may be the best option. These lenses may also not be an ideal fit for the elderly population. Eyes in the geriatric population are often rapidly deteriorating requiring a lens replacement more quickly than would be recommended.
Patients with certain medical histories may also be poor candidates for premium IOL surgery. Some of these conditions include:
Advanced macular degeneration
Anterior basement membrane dystrophy
Fuch’s dystrophy
Weak zonules
Glaucoma
Post-refractive surgery patients
This list is not comprehensive, so it’s important to consult with your physician and bring a detailed medical history for their review.
Finally, patients may also want to consider their careers when weighing the value of this surgery. Patients who are required to read on computer screens for extended periods of time (i.e., print editors, office jobs) may be ideal candidates.
In contrast, individuals that require long-distance acuity like truck drivers, pilots, or even photographers may find that some of the issues with these lenses are not suited to their needs. Individuals often complain of “halos” during the night when looking toward a light, glare, or general acuity issues at longer distances.
Further Consideration
While premium IOLs do have some limitations, they offer an excellent choice for many individuals. However, it is important to meet with your eye care professional to fully discuss all of the available options to find your best fit as well as to make sure that you understand all of the potential risks and restrictions that this operation poses.
EyePromise
We all want to enjoy healthy eyes and clear vision for as long as we possibly can. Fortunately, there are things that we can do to help make this possible. It’s easy to think that protecting our eyes from obvious harm, such as the harsh effects of UV light or potential injury during an activity like welding or woodworking, is enough. However, there are many other things that we can do to keep our eyes functioning well for as long as possible. This includes taking supplements to help ensure that we get the right nutrition for our eyes to be healthy.
EyePromise offers a range of highly effective and expert-recommended nutritional supplements that are designed to support optimal eye health.
Pediatric Eye Exams
Regular eye exams are important for children since their eyes can change significantly in as little as a year as the muscles and tissue develop. Good eyesight is critical for a child’s life and achievements since success in school is closely tied to eye health. School demands intense visual involvement, including reading, writing, using computers, and blackboard/smartboard work. Even physical activities and sports require strong vision. If their eyes aren’t up to the task, a child may feel tired, have trouble concentrating, have problems in school or have difficulty playing their favorite games which may affect their overall quality of life.
When to Perform a Pediatric Eye Exam?
According to research, a child should have an initial screening between 6 and 12 months of age. After that, routine eye health and vision screenings throughout childhood should be performed in order to help detect any abnormalities as their eyes develop. Then, unless otherwise recommended, every two years thereafter until the age of 18.
For a newborn, an optometrist should examine the baby’s eyes and perform a test called “red reflex test” which is a basic indicator that the eyes are normal. In a case that the baby is premature or at high risk for medical problems for other reasons, has signs of abnormalities, or has a family history of serious vision disorders in childhood, the optometrist should perform a comprehensive exam.
A second eye health examination should be done to infants between six months and the first birthday. This examination includes tests of pupil responses to evaluate whether the pupil opens and closes properly in the presence or absence of light, a fixate and follow test to determine whether the baby can fixate on an object such as a light and follow it as it moves, and a preferential looking test which uses cards that are blank on one side with stripes on the other side to attract the gaze of an infant to the stripes and thus vision capabilities can be assessed. Infants should be able to perform this task well by the time they are 3 months old.
For a Preschooler, between the ages of 3 and 3½, a child’s visual acuity and eye alignment should be assessed. If the child is diagnosed with misaligned eyes (strabismus), "lazy eye” (amblyopia), refractive errors (astigmatism, myopia, hyperopia) or any other focusing problems, it’s important to begin treatment as soon as possible to ensure successful vision correction and life-long benefits.
At School age or upon entering school, the child’s eyes should be screened for visual acuity and alignment. In this age group, nearsightedness (myopia) is the most common refractive error and can be corrected with eyeglasses.
Eye Safety Tips
The eye is a very delicate and fragile part of the body. According to one study on distance vision, about 188.5 million individuals are said to suffer from mild vision impairment, 217 million individuals suffer from moderate and severe impairment while 36 million individuals are blind. For near vision impairment, there are about 826 million individuals suffering. In all, there are about 1.3 billion people living with one of these impairments.
While a lot of people are aware that the eyes are an integral part of the body system, most of them do not pay very close attention to taking care of their eyes and are, in essence, taking it for granted. As the saying goes, “You don't know what you have until it's gone," and therefore, we have decided to take the necessary steps to provide you with information on how to best to take care of your eyesight.
Below are ways to keep your eyes safe:
1. Eat Healthy
Eating a healthy diet is a very integral part of keeping the eyes healthy. Nutrients like lutein, vitamins E and C, omega-3 fatty acids, and zinc may help in preventing eye-related problems like cataracts and macular degeneration. These nutrients can be found in vegetables like collards, kale, spinach, fish like tuna, salmon, and halibut, as well as in beans, nuts, eggs, oranges, pork, and oysters.
Besides eating meals rich in nutrients, it is equally important to eat a well-balanced diet. Obesity can cause diabetes and other medical conditions, leading to blindness or glaucoma. Obesity is also regarded as the chief cause of blindness across the globe which should raise a red flag to watch your weight. You can always visit your doctor to get help with drafting a healthy eating plan.
2. Know your family's medical history
Eye issues are usually hereditary which is why it is important to collect a family history on any diseases that may affect eye health and then report them to your eye doctor. This will help to determine your chances of any future eye conditions as well as come up with an action plan for future eye exams.
3. Avoid Smoking
Smoking, in general, is harmful to your overall health. In regards to your eyes, it can cause macular degeneration, destroy the optic nerve, and cause cataracts. It can even lead to vision loss. Quitting smoking if you already smoke, or better yet, not even starting, will be extremely beneficial to your overall health and wellness.
4. Wear Sunglasses
Sunglasses are more than just fashion accessories, they are vital in protecting the eyes from ultraviolet rays emitted from the sun. UV rays can cause macular degeneration and even cataracts which is why it is important to wear sunglasses that protect against 99% -100% of UV rays.
5. Obey workplace safety precautions
It is important we wear protective eye gears when engaging in sporting activities or jobs that could be harmful to the eyes. Such eyewear includes safety goggles, glasses, and helmets. Most of these protectors are from polycarbonates, which is a much stronger material than plastic.
6. Rest your eyes
Just like our bodies, the eyes also need rest to perform optimally. Depriving yourself of adequate sleep and rest can have an adverse effect on the eyes. During the use of the computer, remember to rest the eyes for at least 20 seconds after every 20 minutes by looking away from the screen. Doing this will reduce eye strain.
7. Visit your eye doctor regularly
Getting regular eye exams is one of the most important things you can do for your eye health. Conditions like glaucoma are much easier to treat if they are discovered early so don’t stay far from your doctor.
First Aid
Eye injuries can happen at any time and it is good to know how to handle such emergencies until you can reach a medical professional.
If you get hit on the eyes, you should put a shield like a Styrofoam cup on the bone of the eyes. Avoid putting pressure on the eye
If something enters your eyes, avoid removing it as it may lead to the tearing of important tissue in the eyes. A Styrofoam cup would also do the job here until you can get to a medical professional.
In the case of a black eye, putting an ice pack on the eye will help to reduce bruising and swelling
If it’s a chemical burn, rinse the eyes with clean water for about 30 minutes, holding your head beneath the tap. While rinsing, keep your eyes wide open, rolling your eyeballs in all directions so as to ensure the water gets to every part.
So give some of these tips a try and remember to schedule regular eye exams. Prevention is always a better alternative to trying to find a cure.
Vision Therapy
Vision therapy is a treatment plan that is intended to develop and improve a patient’s visual skills and abilities, with the goal of making their day-to-day life easier. You may also hear Vision Therapy referred to as VT. Although most commonly associated with children, whose visual skills are still naturally developing, adults can also benefit from vision therapy.
Any patient who does not have the necessary visual skills could find themselves suffering from a range of unpleasant symptoms, including headaches, eye fatigue, stiff neck, and double vision. Fortunately, vision therapy is a simple, painless technique to help patients to enhance their visual skills and overcome any issues that they may have been experiencing.
Skills that can be developed and improved through vision therapy
Vision therapy has been shown to be an effective way of developing and improving the following visual skills, all of which are important for day-to-day life.
Tracking: this refers to the ability to follow a moving object smoothly and accurately with both eyes – such as moving traffic or a ball coming towards you.
Depth perception: this is the ability to judge relative distances of objects and move accurately in a 3D space – for example, being able to walk down a flight of stairs.
Peripheral vision: this refers to the edges of your vision and your ability to assess what’s happening in your peripheral vision while paying attention to something directly in front of you.
Acuity at different distances: this is the ability to see clearly enough to identify and understand objects at both near and far distances.
Fixation: enabling patients to quickly and accurately look at, identify and understand stationery objects one after the other, for example, reading word to word.
Binocular vision: the ability for both eyes to work together in perfect synchronization.
Shifting focus: patients with this skill can look quickly at different distances without momentary blur.
Visualization: a valuable visual skill that enables patients to form and retain images in their head.
What to expect from a vision therapy appointment?
Vision therapy is generally conducted as an in-office treatment, under the close supervision of your eye doctor. Each vision therapy treatment plan is personalized; tailored to the specific individual needs of each patient. Most patients can expect to schedule hour appointments once or twice a week. You may also be given specific exercises to complete at home, which will support the progress that you are making during your in-office appointments. The components of Vision Therapy Treatment are non-invasive and drug-free, making VT suitable for the vast majority of patients, regardless of their age, health and history. For many people, vision therapy is a safe alternative to conventional eye surgeries.
There are various techniques that can be involved in vision therapy. These include, but aren’t limited to:
Prisms
Patches
Occluders
Therapeutic lenses
Exercises
The use of tools designed specifically for use in vision therapy exercises
By attending regular vision therapy appointments, patients can see an improvement in their vision, visual comfort and experience an overall improvement with the ease in which they use their eyes for daily activites.
Glaucoma Treatment
If you’ve been diagnosed with glaucoma, you’re probably already familiar with the typical options in glaucoma treatment – eye drops, laser treatment or traditional surgery. While these are certainly effective, especially when glaucoma is diagnosed early, researchers have been working hard to offer new glaucoma treatments. Their goal is not only to improve outcomes but also reduce the treatment’s side effects and frequency of use.
What is the Goal of Glaucoma Treatment?
Before we dive into the new options, it’s important to understand the goal of any glaucoma treatment. At present, glaucoma is not curable. However, treatment can significantly slow the progression of the disease. Glaucoma damages your eye's optic nerve. Extra fluid builds up in the front part of your eye (cornea), which increases the pressure in your eye. Reducing this pressure is the primary objective of any glaucoma treatment. This is often referred to as intraocular pressure or IOP.
What are the Limitations of Standard Glaucoma Treatments?
Eye drops for glaucoma treatment seem like an easy option but there are several challenges that can reduce its effectiveness. It can be difficult to get all the medicine in the eye, especially for older adults with less of a steady hand. In addition, since it must be applied daily, individuals may forget. Since the drops have no perceivable benefit because early stages of glaucoma have no symptoms, patients might make it a lower priority which is understandable since it may also have unpleasant side effects like burning, red eyes.
Beyond eye drops, laser surgery is a less invasive option. The laser opens clogged tubes and drains fluid. It can take a few weeks to see the full results. If laser surgery or drugs don’t relieve your eye pressure, you may need a more traditional operation. You would have to go into the hospital and will need a few weeks to heal and recover. Although usually effective, glaucoma surgery can make you more likely to get cataracts later on. It can also cause eye pain or redness, infection, inflammation, or bleeding in your eye.
What are Recent Advances in Glaucoma Treatment?
Alternatives or Improvements to Eye Drops
The Glaucoma Research Foundation reported several new developments on the horizon. These technologies focus on reducing patient error in applying eye drops which would make the medication more effective and improve the quality of life for the patient. Here are some of the products underway:
A polymer, like a contact lens, would contain the drug; it would sit under the eyelid and release the medication over several months
Microneedles would inject medication into a specific spot to be most effective
Implantable extended-release devices using engineered highly precise microparticles and nanoparticles
Polymer-based intraocular delivery technologies that would allow customizable sustained release
Drops that allow the medication to get into the eye more easily
Tear duct plugs that release medication
In addition, people with glaucoma who take more than one eye drop per day are beginning to see those medications available as a single, combined eye drop. New products include Cosopt (timolol and dorzolamide), Combigan (timolol and brimonidine) and Simbrinza (brinzolamide and brimonidine).
Ortho K
Many patients come to us every day struggling to get through their daily lives with their current choice of vision correction. Some have eyeglasses that do not sit properly on their face or feel that their peripheral vision is hindered by the frames. While contact users may find the lenses uncomfortable or have them fall out at inconvenient times. For these patients, we are pleased to offer orthokeratology, or Ortho-K, a revolutionary way to help you see clearly throughout the day without having to wear glasses or contacts and without having to get laser eye surgery.
What is Ortho-K?
Generations ago, eye doctors knew that the tissue in the eye was soft and somewhat malleable. This knowledge caused them to wonder if they could push the eye back into the proper shape, would an individual be able to see clearly even if they were not wearing their prescription lenses. With the development of gas permeable contact lenses, a few eye doctors began to notice that their patient’s prescriptions did not change as rapidly as previously noted and that they appeared to be able to see correctly even when they were not wearing their contacts.
From these early discoveries, the world of Ortho-K was born. Ortho-K is a special treatment to help patients see clearly even when they are not wearing a prescription lens. Instead, a special gas permeable contact lens is placed into the eye each night before bed and the lens gently pushes the eye into the proper shape while you sleep. In the morning, you can remove the lenses and still see clearly throughout the day. Some patients can even see clearly for up to three days after wearing them for just one night!
Who Should Consider Ortho-K?
There are a number of issues that our patients can have with prescription lenses. If you have one of the following conditions or concerns, call our office today to schedule an appointment.
Allergies to the materials in contact lenses
Dry eye that is made worse by wearing prescription lenses
Dirt or other debris that gets under contact lenses
You play sports and do not want to worry about glasses or contacts
The ability to wake up at night and see clearly
A general dislike of glasses or contacts
How Long Does It Take?
Once you receive your custom Ortho-K contact lenses, it will take anywhere from one to four weeks to fully see all the benefits to your vision that they will provide. However, some of our patients find that their vision has improved after only wearing their lenses for a single night! During the first few days, you may also still need to wear prescription lenses to see clearly enough to drive or get through your normal day, but that is generally quickly resolved. Also, some patients experience some mild discomfort for the first few nights, but as your eyes adjust over a few days, you should no longer be bothered by the feel of your lenses. Is the Procedure Safe? Orthokeratology was approved by the Food and Drug Administration (FDA) in 2002. The procedure is considered safe, effective, and reversible. However, there are some side effects associated with Ortho-K. Most of these side effects are a result of improper cleaning of the lenses that can lead to a minor infection. These infections are usually remedied fairly quickly with the use of antibiotic eyedrops.
Overview
If you are sick and tired of wearing contact lenses or glasses every single day and would like an alternative way to correct your vision, consider trying Ortho-K. If you would like more information on Ortho-K, please call our offices today and see how we can improve your everyday life.
Seasonal Allergies And The Eyes
Seasonal allergies is a medical condition similar to other forms of allergies that occur when the body's immune system reacts to an external material in the environment during seasonal periods when plants and trees are pollinating. Seasonal allergies have a tremendous effect on millions of individuals annually causing a negative effect on eyesight. Seasonal eye allergies cause the eyes to become itchy, watery and red which in medical terms is referred to as allergic conjunctivitis. There are many allergens that can make our eyes go itchy and very red including dust, pollen, and smoke. These allergens, however, vary from one person to another. For example, while dust can cause itchy eyes for me, it might not be the same for you as it all depends on our immune system and the way it reacts against such substances.
When something is regarded as a dangerous substance by the eye, a chemical response is elicited to fight against the allergen which is what leads to the itchiness, redness, and soreness in the eyes. These reactions are usually a result of a change in seasons, mostly occurring in the spring when plants and trees are pollinating and during the fall when the ragweed plants are pollinating.
Seasonal Allergies Effect on the Eyes
As we mentioned earlier, allergens affect people differently, but there are general ways in which everyone reacts. You would know an individual is suffering from allergies through the following symptoms.
Teary eyes
Since the eyes perceive substances like dust, smoke, pollens as harmful to the normal conditioning of the eyes, there is an automatic release of water in order to clean the eyes which is more of a defense mechanism against these foreign items.Swollen eyes
After the entry of these foreign items, it is very natural to feel itchy and want to scratch the affected eyes. During the scratching, the skin covering the eyes would become swollen due to continuous friction.Dry eyes
Dry eyes occur most times during winter seasons, not because of allergens like dust or pollen, but whenever there is extreme cold or snow. This causes the eyes to become dry which leads to soreness and redness.Itchy Eyes
Allergens are carried by air and could end up in your eyes at any time. A reaction to these allergens would cause your eyes to feel irritated from the inside and would create the urge to then scratch your eyes in an attempt to provide some relief.Red Eyes
Redness of the eyes is usually accompanied by other symptoms such as itchy eyes which cause the eyes to become swollen and very red. There are also capillaries inside the eyes that can become red whenever one is faced with an allergy.
Prevention
It is nearly impossible to prevent allergens due to the fact that they are carried around by air. There are, however, some things that can be done by you to help reduce your chances of being exposed to allergens. One of the first precautions is to remain indoors on windy days since more allergens are carried around at a faster pace. If it is necessary to go out, be sure to wear a pair of sunglasses that provide adequate coverage for the eyes. Furthermore, wearing pollen masks and/or sunglasses when working in the yard could help to prevent anything from blowing into your eyes.
Treatment
Whenever you are suffering from allergies, be sure to stay hydrated, use any doctor recommended eye drops you may have to help reduce irritation, and if you use contact lenses, switch to a pair of glasses to add some extra protection as well as prevent further eye discomfort. Lastly, try to avoid scratching your eyes as much as possible to prevent any additional complications.
iDesign Custom Lasik
If you thought that just laser eye surgery was impressive, then be prepared to be astounded by the arrival of iDesign custom Lasik. iDesign is the most advanced wavefront-guided laser treatment available. The system creates a uniquely accurate measurement of the entire optical system that can be relied upon completely without any guesswork. This is then used to create a highly detailed topography or map of your eye, making it easier for your surgeon to pinpoint the areas that need addressing with pinpoint precision.
How accurate is iDesign?
iDesign is extremely accurate due to its diagnostic equipment that is able to determine 1,257 different micro eye prescriptions. Each one of these will measure the eye prescription to 0.01 of a dioptre strength – 25 times more than what a regular prescription for glasses or contact lens prescription is measured to.
Who is iDesign suitable for?
While iDesign Custom Lasik can benefit almost any patient with refractive problems, it is particularly beneficial for people who have unusual corneas or have had eye surgery in the past.
Is it painful?
Laser eye surgery is generally considered a pain-free procedure by the majority of patients. Anesthetic eye-drops are used to numb the outer area of the eye during the course of the surgery. Once these have worn off, some patients do experience some mild discomfort during the days following the procedure, but over the counter pain relief is usually sufficient to relieve this.
Lipiflow
Dry eyes are one of the most common conditions that can affect our eyes and is estimated to affect millions of Americans. As you’ve probably guessed, dry eyes occur when tears fail to provide enough natural lubrication for the eyes to be comfortable and healthy. Exactly what causes dry eyes can vary significantly, from side effects from medications to prolonged computer use. What is clear is that while the condition isn’t sight-threatening, it can make day to day life much harder than it needs to be. Fortunately, there are treatments that can help, and arguably one of the most effective is Lipiflow.
What is Lipiflow?
Lipiflow is a new technological solution that addresses the underlying cause of your dry eyes, rather than simply treating the symptoms. It is most effective at helping patients whose dry eyes are caused by meibomian gland dysfunction – a condition characterized by problems with the way that the meibomian glands produce the oil that forms an essential part of our tear film. The meibomian glands can become less productive, or in some cases, even blocked by hardened oil deposits. This prevents the oil from reaching your tear film, making it less effective. Lipiflow targets the meibomian glands, warming them to break down oily blockages and massaging your eyes to make sure that the oil, and then the tear film, is evenly dispersed. This helps to combat the symptoms associated with dry eyes, which can include:
Eye fatigue
Dry, scratchy and uncomfortable eyes
Blurred vision
Sensitivity to light
Difficulty wearing contact lenses
Your eye doctor will be able to advise you if Lipiflow has the potential to be a suitable solution for your dry eyes.
What to expect from Lipiflow treatment?
Lipiflow treatment is a simple, painless process that is performed in the comfort of your eye doctor’s office. There is no need for anesthetic. Once you are settled in your chair, your eye doctor will open the sterile, single-use applicators which are placed over your eyes. These are connected to a machine that causes the inner eyelids to heat to approximately 42.5°C to, while simultaneously placing gentle pressure on the outer eyelid surfaces. Lipiflow takes around 12 minutes per eye, during which time you can relax. You can even listen to music if you’d like to. There is no downtime, and patients can return to their usual activities right away. It takes around 3 days for patients to begin to see an improvement in their dry eye symptoms, although they may require further treatment in the future to maintain them. Optimal results are usually achieved around 6 to 8 weeks following your Lipiflow treatment.
For more information about Lipiflow, or to schedule a consultation to talk about this treatment for dry eyes, please contact our office.
Why Should You Consider Eyelid Rejuvenation
Eyelid rejuvenation surgery is a medical procedure that is designed to reduce the appearance of bagginess from the lower eyelids and sagging from the upper eyelids. This operation is often used for cosmetic surgery to reduce the appearance of aging.
This surgery can also be considered when the eyelids are interfering with a patient’s ability to see. Sometimes a sagging upper eyelid can partially obscure the eyeball, interfere with a person’s ability to look in certain directions or interfere with their peripheral vision.
Why Do My Eyelids Sag?
As our skin ages, it often loses its elasticity. This doesn’t allow the skin to rebound back to its original shape and we see the appearance of wrinkles and bulges that aren’t due to weight gain. While these wrinkles can occur all over the body, they typically first appear in the face and eyes. Any additional skin on or near the eyelids can cause the eyelid to sag or droop over the eyelashes and into the frame of vision.
The eyelids also contain some fat to protect and cushion the eyeball. The fat is held in place by a thin membrane. As we age, the membrane can weaken and will no longer keep the fat in place. This fat can create bulges in the upper and lower eyelids.
What Can I Do About Eyelid Sag or Bulging?
There are several non-surgical treatments on the market to help treat sagging skin or reduce the appearance of wrinkles, but it is important to use additional caution when applying any product near the eyes. Always make sure that the product is designed to be used in the predetermined area. If you have questions about a specific product, you should contact your health care provider.
Many individuals find that non-surgical options don’t have enough or any effect on their eyelids. In these instances, they can consider working with a licensed medical professional to weigh their options. Eyelid rejuvenation (blepharoplasty) is also commonly called an eye lift.
There are several different methods for achieving your desired results. Typically, an incision is made into the eyelid, and then the excess skin or fat cells are removed by laser or scalpel. Additionally, your surgeon may suggest that you also get laser resurfacing done in combination with your surgery.
What to Expect
Eyelid surgery can be done in a local office or a surgery center. If you are completing the operation in an office environment, you can probably expect that you will be treated with a local anesthetic and an oral sedative. If you are in a surgery center, it’s likely that you will receive an intravenous anesthetic. The surgery takes about two hours to complete if you are getting all four eyelids done (upper and lower lids). When you are getting all four eyelids corrected, the surgeon will likely opt to work on both upper eyelids first and then move to the lower eyelids. While the upper eyelids will have three to six stitches, the lower eyelids may not have any. The stitches should remain in place for three to six days.
Tonometer
A tonometer refers to the equipment that is used in tonometry – a test that measures the pressure inside your eyes, also known as intraocular pressure or IOP for short. Tonometry is rarely performed at your average comprehensive eye exam unless you are at high risk of or have been already diagnosed with glaucoma. Fortunately, tonometry can be used to detect changes in eye pressure before they cause any symptoms, enabling prompt action to be taken before your vision is affected.
About Glaucoma
Glaucoma is a common eye condition that occurs when the optic nerve, which connects the eye to the brain, becomes damaged. It’s normally caused by fluid building up in the front part of the eye, which causes the pressure inside the eyes to build. As the pressure increases, the optic nerve becomes increasingly damaged, and this prevents messages from being transmitted between your eyes and brain effectively. As a result, the patient’s vision becomes compromised. Without treatment, the level of vision loss will continue to increase. Unfortunately, any vision that has been lost as a result of glaucoma cannot be restored.
Most of the time, glaucoma develops very slowly which means that many people don’t realize that they are affected until some damage to their vision has already occurred. However, occasionally glaucoma can develop quickly, and symptoms do occur.
These can include:
Red eyes
Intense headaches
Tenderness around the eyes
Eye pain
Seeing rings/halos around lights
Blurred vision
Nausea and vomiting
If you notice any of these symptoms, it’s important that you make an appointment with your eye doctor right away so that you can be assessed. You are likely to have a tonometry test as part of this assessment.
What to expect from tonometry testing
There are various methods of tonometry testing, but many eye doctors use either Goldmann tonometry, which is the conventional technique to measure eye pressure, or electronic tonometry.
Goldmann tonometry testing is carried out using the Goldmann applanation tonometer, which is attached to a slit lamp microscope. This requires anesthetic eye drops to be used which numb your eyes, before a small probe is pressed gently against the eye, indenting the cornea. The pressure that the cornea pushes back onto the tonometer is what is measured to give your IOP reading. Electronic tonometry is where a handheld, mobile device is gently and quickly applied to the cornea to check the pressure, providing an accurate reading. Some eye doctors also offer non-contact tonometry which is where a puff of air is used to flatten the cornea, although this is reported to be less accurate than the Goldmann technique.
If you would like to find out more about Tonometry testing, please call our office to speak with our dedicated eyecare professionals.
What to Expect During an Eye Exam
The parts of a comprehensive eye examination vary according to the patient's age, date of last exam, and other factors. Not all parts of the eye exam may be needed or performed, but the first part of the eye exam will include documenting medical history. Here are some eye and vision tests that are likely to be encountered during a comprehensive eye exam:
Visual Acuity Tests
Visual acuity tests measure the sharpness of vision and are usually performed using a projected eye chart to measure the distance visual acuity and a hand-held small acuity chart to measure the near vision (for reading).
Color Blindness Test
A screening test that checks the color vision is often performed early in a comprehensive eye exam to rule out color blindness.
Cover test to check eye alignment.
A test used to assess strabismus or a more subtle binocular vision problem that could cause eye strain or amblyopia (lazy eye).
Ocular Motility (Eye Movements) Testing
Ocular motility testing is performed to determine how well eyes can follow a moving object and/or quickly move between and accurately fixate on two separate targets.
Stereopsis (Depth Perception) Test
This is used to test perception of depth and 3-dimensional structure obtained on the basis of visual information deriving from two eyes by individuals with normally developed binocular vision.
Retinoscopy
This test is used to estimate which lens powers will best correct distance vision. Based on the way the light reflects from the eye, the doctor is able to obtain an approximation of the eyeglass prescription. This test is useful for children and patients who are unable to accurately answer the doctor's questions.
Manual refraction with a phoropter.
This is the test used to determine the exact eyeglass prescription.
Demodex
What Is Demodex?
The Demodex mite is a type of parasite that lives on humans and can reside in hair follicles and sebaceous glands. These mites are arachnid (eight-legged) and invisible to the naked eye, varying in size from 0.1mm to 0.4 mm long. They typically live on the face and in the hair follicles of the eyebrows, eyelids, roots of the eyelashes, facial hair, and around the ears and are associated with various skin problems of the eyes and face, such as blepharitis and acne rosacea.
Demodex can affect humans at any age, but their presence increases in prevalence with increasing age. Immunity compromised patients such as diabetics, patients on long-term corticosteroids or chemotherapy, or patients who have HIV/AIDS also have increased risk and prevalence of Demodex infection. Usually, when the immune system is weakened and the parasitic population has colonized, this disease can badly damage the skin.
How Can Demodex be Transmitted?
For transmission of mites from one person to another, direct contact of hair and sebaceous glands on the nose, or dust containing eggs is required. Since the disease processes begin when there is an overpopulation of Demodex, the vast majority of cases of mites go unobserved and don't show any adverse symptoms. However, in certain cases, the mite populations migrate and multiply in the eyelashes.
What Are The Types of Demodex?
There are two existing types of Demodex mites: the longer kind, Demodex folliculorum, which live in the hair follicles and the short ones, Demodex brevis, which live in the sebaceous (oil) glands in the skin.
What Are The Symptoms of Demodex?
In the early stages, there are often no noticeable symptoms, but if left untreated Demodex can progress. Symptoms vary among patients and may include dry eye, red eyes, severe itching along the eyelid margin and eyebrow, especially in the morning, eyelid irritation, burning sensation, foreign body sensation that seems to originate beneath the eyelids, heavy lid, and blurry vision. One of the earliest signs of mite infestation is cylindrical dandruff (CD), which is the accumulation of fine, waxy, dry debris that collects at the base of the lash and extends up to 2 mm along the length of the lashes and is most noticeable on the upper lashes.
Comprehensive Eye Exam
If you’ve had a vision screening recently, you might say, “My vision is fine! I don’t need a comprehensive eye exam.”
But a vision screening provides a limited perspective on the overall health of your eyes. It’s a bit like getting your blood pressure checked and not getting the rest of your annual physical. You’ll have useful information, but it’s not the whole picture.
What are the Limitations of a Vision Screening?
Vision screenings only test your ability to see clearly in the distance. This is called visual acuity and is just one factor in your overall vision. Others include color vision, peripheral vision, and depth perception. The screening also doesn’t evaluate how well the eyes focus up close or work together. Most importantly, it doesn’t give any information about the health of the eyes.
Vision screenings are conducted by individuals untrained in eye health.
Vision screenings are offered in many places – schools, health fairs, as part of a work physical or for a driver’s license. Even if your physician conducts the screening, he/she is a generalist and only has access to a certain amount of eye health training. Most individuals don’t have the tools or knowledge to give you a complete assessment of your vision or eye health.
Vision screenings use inadequate testing equipment.
In some cases, a vision screening is limited to an eye chart across the room. Even when conducted in a physician's office, they won’t have the extensive testing equipment of an eye doctor. They also won’t be aware of nuances such as room lighting and testing distances all of which are factors that can affect test results.
What are the Benefits of a Comprehensive Eye Exam?
Comprehensive eye exams evaluate all aspects of your vision and eye health.
The comprehensive eye exam looks at your eye externally and internally for any signs of eye disease, then tests your vision in a variety of ways.
Understanding Computer Vision Syndrome
Just a few decades ago, computer vision syndrome (CVS) was not known or understood. However, with an increase in the role of computers in our lives, it has become an increasingly common issue. Researchers believe that 50-90% of people who use computers in their daily lives have experienced CVS to some degree. The amount of time that many people stare into a computer screen is increasing, which puts significant strain on our eyes.
CVS is not considered a single specific problem, but a suite of issues. And with the increased use of school computers, tablets and smartphones, children are also becoming more susceptible to CVS.
This syndrome is similar to many other repetitive motion type conditions such as carpal tunnel syndrome. Problems can start because as we are reading text on a screen, our eyes move in a repetitive motion throughout the day. Once the issue has started, continuing the same behavior can worsen any symptoms. While reading alone uses the same motion, digital screens add flicker, contrast, glare, and light that all put additional strain on our eyes.
Issues may also be accelerated if you should be wearing some type of corrective lens, but don't, and are therefore putting additional strain on your eyes.
Aging can also speed up the progress of these issues. Around the time that people turn 40, the lenses of the eyes begin to harden due to a disease called presbyopia, which affects your ability to see closer objects.
What Happens if I have CVS?
There is currently no proof that CVS causes long-term vision impairment or blindness. Continuing to use a computer or any other type of screen can continue to be an annoyance or reduce your ability to see properly. Some of the warning signs of CVS are:
Blurred vision
Double vision
Red or dry eyes
Headaches
Neck pain
Back pain
Eye Irritation
If you don’t properly treat CVS when these symptoms occur, you may begin to notice that you suffer from a decrease in overall quality of life or job performance.
Considering Your Face Shape When Choosing Eye Glass Frames
When it’s time to select a new pair of eyeglasses, it can be challenging to find the frame that feels the best for you. Eyeglass makers have become increasingly aware of their clients’ desire to customize frames as well as offer a variety of colors, designs, and frame shapes. Understanding more about your face shape and the types of frames that would look best on you can help to reduce the amount of time you spend trying on frames that don’t complement your face shape. Here are a few useful tips to help you find glasses best suited for your face shape.
Face Types
While there are thousands of different frame shapes, there are only seven different face shapes.
Round
This face type is as wide is it is long. There are no specific or well-defined angles to this face type. Most people with this facial type look for frames that will elongate their face in order to draw out their natural features as well as give their face a thinner appearance. A good choice is often to select a frame that is angular and narrow.
Heart
If you can imagine the shape of a traditional heart, this face shape is easy to identify. The top 1/3 of the face is wider while the rest of the face tapers to a narrow chin. Individuals with this face shape will often seek frames that are wider at the bottom of the lens. This helps to balance the face and give the appearance of a narrower face at the top. Another great fit for this face type would be rimless frames.
Base Down Triangle
This face type contains a wide jaw and cheekbones but is narrow at the forehead. Cat-eye type frames are great for this face type, as are frames that are heavier near the eyebrow to provide more balance.
Diamond
This face type is the rarest. The diamond face is like the base-down triangle but differs because it has a narrow chin, thus appearing like a diamond. When selecting eyeglasses, look for oval-shaped frames, or frames that have more detail along the brow line.
Oblong
This face type looks like an oval, but these individuals have a straight cheek line. This face is fuller than it is long. Frame types that add some depth are ideal for this face. This can be done by finding frames that have decorative pieces along the temples or that have more depth with a reduced width.
Oval
Oval faces are the most common face type. They are considered to have balanced proportions so that most frame types will work well. An oval face is longer than it is wide and includes plump cheekbones. Walnut shaped eyeglasses are an ideal choice, but frames that are as wide or wider than the broadest part of your face would work as well.
Square
These individuals have a broad forehead and jaw that gives the appearance of the face having equal and straight sides. These face types usually do well with narrow or oval-shaped frames which will help to soften their features.
Additional Tips
Your hair color may play a role in the best frame color for you. Individuals with warm hair colors (brown or black hair) do best to choose a lighter colored frame to add contrast. People that have hair on the lighter end of the spectrum can pick just about any frame color that they would like and may look to other features like eye color or skin tone to help make their decision.
Skin tone has the opposite effect from hair color on the best choices for the frame color. Those with lighter skin hues do best with similar frame colors, and those with warmer skin tones can pick and choose options that they enjoy the most.
Above all else, you should pick a frame that you like best. There may be additional factors to consider when choosing the right frame for you, but perhaps the most important factor is your overall happiness and comfort.
How Your Eyes Change with Age
As our bodies age, it is normal to notice that there are decreases in our ability to complete certain functions that may have been natural for us in our youth. Just like our physical strength, the strength of your eyes can also weaken over time.
Several different factors influence how each of us will experience aging. Your genetics can play a pivotal role. Understanding your family history and making sure to communicate this with your health professional can be a great way to monitor changes and spot early signs and symptoms. Exposure to certain chemicals or environments or specific trauma to our eyes can also have an impact on how our eyes age. While the eyes can often recover from traumatic injury or exposure, they may still have a detrimental effect on your vision as you age.
Knowing what age you start to have an increased risk of certain diseases or eye conditions can help you to be prepared when you meet with your optometrist. Here are some of the most common ailments that people experience when they age.
Presbyopia
Once you are over 40 years old you may experience a loss in vision at close range. Presbyopia is a normal condition that occurs due to the hardening of the lens in your eye. In the early stages, you can often compensate for small changes to your vision, but as the condition progresses, you will likely need a corrective lens, or choose a surgical procedure. such as Lasik, corneal inlays, refractive lens exchange, and conductive keratoplasty.
Cataracts
Cataracts are technically a disease of the eye. However, they are so frequently seen in patients as they age, that they are classified as a normal part of aging. While almost half of the population over 65 have cataracts, that number increases even more by age 70. While it can be frightening to begin losing your vision, cataract surgery is extremely successful and can restore up to 100% of the lost vision. If you notice even small changes to your vision, it is smart to talk to your doctor. Cataract surgery is best performed when the cataracts are small and can be more easily removed.
Macular Degeneration
This disease is the leading cause of blindness in senior citizens in the United States.
Glaucoma
The risk of developing glaucoma generally begins when you are in your 40’s with a near one percent chance and increases throughout the decades with a twelve percent by the time you are in your 80’s.
Diabetic Retinopathy
Individuals who have diabetes may be affected by diabetic retinopathy. This disease occurs when blood sugar levels are elevated for an extended period that causes damage to the eye. This damage may lead to permanent vision loss. Americans with diabetes over the age of 40 are at an increased risk, with about 40 percent of people with diabetes over this age displaying some degree of diabetic retinopathy.
Scleral Lenses
Contact lenses come in a variety of shapes and styles to suit the range of needs for individual patients. What this means is that there is almost certainly a type of contact lens that will both feel comfortable for you and improve your vision.
Some types of contact lenses are known as speciality lenses. This is because they are designed specifically to overcome some eye issues which may prevent a patient from wearing the most common and generic styles of contact lenses. In fact, speciality contact lenses have transformed the vision options of many patients who would otherwise have only had the choice between wearing glasses or undergoing laser vision correction. There are numerous types of speciality contact lens, including scleral lenses.
What are scleral lenses?
Scleral contact lenses get their name from the fact that, unlike regular contacts, they vault over the entire corneal surface and rest on the white part of the eye, which is called the sclera. This makes them larger than standard contacts, which in turn provides a variety of benefits. Their size makes them easier to handle and more stable when on the eye, which in turn provides the patient with sharper and more reliable vision. They are also less likely to become dislodged and come out.
Scleral contact lenses are also gas permeable, which means that oxygen can pass right through them and reach the surface of the eyes. This is important for comfort, particularly for patients who experience dry eyes. The gap that is created between the back of the contact lens and the front surface of the eye can also trap tear film, acting as a fluid reservoir which will keep the eyes moist and healthy.
Types of scleral lenses
Within scleral lenses there are several different sizes to choose between. These are based on where the lenses meet the surface of the eye and are as follows:
Full scleral lenses: the largest type, they provide the greatest amount of clearance between the cornea and lens and rest on the outer sclera.
Mini scleral lenses: the mid-size variety, make contact with the eye on the anterior sclera.
Semi-scleral lenses: although larger than conventional lenses, they are not huge, and the edge of the contact lens rests on the junction between the cornea and the sclera.
Your scleral lens provider will be able to make a recommendation as to the correct size for you, which will be based on your individual requirements.
Who are scleral lenses recommended for?
Although technically anyone can wear and benefit from scleral lenses, they are a particularly good option for patients who have eye conditions or irregularities that for which regular contacts are not suitable. This includes patients with:
Dye eye syndrome. Contact lenses float on a fine layer of tear film, which keeps them comfortable and in position. Patients with dry eye syndrome either do not have enough natural tear film, or what they do have drains away too quickly. This can
make wearing regular contact lenses difficult and uncomfortable. However, the design of scleral lenses keeps moisture on the surface of the eyes, eliminating some of the effects of dry eyes. This makes scleral lenses a great choice for patients with dry eyes.
Irregular corneas. The cornea is the clear dome that covers the front part of the eye and many people have a cornea that is a slightly, or significantly, irregular shape. This causes light to be refracted incorrectly when it enters our eyes, triggering vision problems. Issues arising from irregularly shaped corneas cannot be completely corrected using glasses or conventional contact lenses. Therefore, scleral lenses, which provide sharper and more accurate vision, are recommended.
For more information about scleral lenses, please do not hesitate to call our expert eye care team.
Contact Lens Exam
If you’ve never worn contact lenses before, it can seem a bit intimidating. After all, you’re inserting something into your eye! Let’s ease your mind about the first step – your contact lens exam. This post will walk you through what’s involved in a contact lens exam and what you can expect every step of the way.
It begins with a comprehensive eye exam.
Your eye doctor will first determine your overall eye health and vision. This includes a discussion of your health history and then a series of standard eye tests. These tests will evaluate eye focusing, eye teaming, depth perception, color vision, peripheral vision, and the response of your pupils to light. The doctor will also measure your eye’s fluid pressure to check for glaucoma, evaluate your retina and optic nerve, and test your vision with different lenses to assess whether contact lenses can improve your vision.
Then, a discussion about your contact lens preferences.
If contact lenses are appropriate for you, it’s time to talk about your contact lens preferences. For example, do you want to enhance or change your eye color? Would you prefer daily disposable lenses or overnight contacts? Ask about the benefits or drawbacks of each, so that you make the best decision. If you’re over 40, your doctor will likely discuss age-related vision changes and how contact lenses can address these issues.
Next, the eye doctor will conduct eye surface measurements.
Contact lenses require precise measurements of your eyes to fit properly. Using an instrument called a keratometer, your doctor will measure the curvature of your eye's cornea, the clear front surface of your eye. Next, the size of your eyes pupil is measured using a card or ruler showing different pupil sizes which is held next to your eye to determine the best match.
You may also need a tear film evaluation.
If you have dry eyes, your eye doctor will perform a tear film evaluation to measure the amount of tear film on the surface of your eye. If your tear film is insufficient or you have chronic dry eyes, contact lenses may not be a good option for you. However, some newer contact lenses deliver moisture to the surface of the eye, making them a better choice for individuals with dry eye issues.
It's time for the contact lens fitting.
The final step is to fit you with a trial pair of contact lenses. Once inserted, your eye doctor will examine the lenses in your eyes to ensure a good fit. He/she will check the alignment and movement of the lenses on the surface of your eye and if the fit looks good, the last step is to ensure the prescription is correct with a few more tests.
Now it’s your turn to test it out.
Your contact lens exam is over, but you’ll need to come back. Your doctor will usually have you wear the trial lenses for a week. After that, you’ll have a short follow-up exam to confirm that the lenses are working well for you and you can then order a supply of contact lenses. If this is your first contact lens exam, don’t worry. Choose a qualified optometrist and they’ll answer all your questions as you go. Just be sure to let them know you’re interested in contact lenses so that they know to allow for extra time in your appointment for the consultation and any specialized tests.
Diabetic Related Eye Exams
You have almost certainly heard of diabetes, which is one of the most common chronic health conditions in the United States with an estimated 100 million adults currently living with diabetes or pre-diabetes. This metabolic disorder occurs when the body is no longer able to regulate its own blood sugar levels and requires intervention to keep them stable. Most people are aware that diabetes can have serious consequences for our health. However, you may be surprised to learn that it can also influence our vision. This is because patients who are diabetic can go on to develop a complication that is known as diabetic retinopathy. Without prompt treatment, diabetic retinopathy can cause permanent vision loss. It is for this reason that patients who suffer from diabetes are asked to attend regular diabetic-related eye exams.
What is diabetic retinopathy?
For us to be able to see clearly, our eyes need to be healthy and functioning perfectly. The most important component of our eyes are the retina. Found at the very back of the eye, the retina is a patch of light-sensitive cells that have the job of converting the light that passes into the eye into messages that are passed up the optic nerve and into our brain. Our brain then receives them and tells us what we can see and how clearly we can see it.
The retina relies on a continuous supply of blood, which is delivered using a network of tiny blood vessels. Over time, having continuously high blood vessels can damage these blood vessels causing a leak of blood and other fluids onto the retina. If this happens, scarring may occur which could compromise the quality of your vision.
Am I at risk of diabetic retinopathy?
Technically, anyone who suffers from diabetes, whether it be Type 1 or Type 2, could be at risk of developing diabetic retinopathy. However, the condition is more likely in certain situations. These include if:
your blood sugar levels are uncontrolled or poorly controlled
you have a long history of diabetes
you have high blood pressure (hypertension)
you suffer from high cholesterol
you are pregnant
Regular diabetic-related eye exams will enable your eye doctor to monitor your condition and ensure that any signs of diabetic retinopathy are detected and acted upon immediately.
What to expect from diabetic-related eye exams?
The process of a diabetic eye exam is very simple and straightforward. In fact, in most instances, it is included within the other elements of comprehensive eye exam and you may not even realize that you have had a specific test to check for diabetes-related complications.
Diabetic eye screening is non-invasive. You will be given eyedrops which will blur your vision. These may sting a little when they are administered, but this will pass within just a few moments. Once your vision is blurred, you will be asked to rest your head onto a device and stare down a lens. This leads to a camera which will take images of the backs of your eyes so that your eye doctor can assess the structures, which include the retina, for any abnormalities. You will see a flash when each image is taken, but at no point should you be in any pain.
In addition to the images of the back of your eye being taken, you will also be given a visual acuity test. This is where you will be asked to read letters off a chart a short distance away, as well as reading from a card held in front of you.
The information that your eye doctor will obtain from your examination will be able to tell them if you are experiencing any of the signs of diabetic retinopathy. If so, they will discuss the best way to get your condition under control. This could involve a combination of elements, including controlling your diabetes more effectively, taking medications or more invasive treatment to preserve your vision. Your eye doctor will give you more specific information based on your individual circumstances.
If you have further questions about diabetic-related eye exams, please contact our knowledgeable eye care team.
TempSure Envi
Whether people like it or not, fine lines and wrinkles go hand in hand with the aging process. However, they typically appear sooner and look worse for those who spend time in the sun. Fortunately, TempSure Envi offers a solution that improves the skin’s appearance and health.
Instead of having invasive surgery, experts in the field of aesthetics can offer their patients something better. Not only is TempSure Envi non-invasive, but it’s also safe and effective. Simply put, it provides optimal improvement without any pain or discomfort.
Beyond Fine Lines and Wrinkles
Eliminating fine lines and wrinkles is just one of many benefits associated with TempSure Envi treatments. This same treatment works incredibly well to reduce the appearance of cellulite. Overall, it smooths skin, making it look more youthful.
However, even leading ophthalmologists and optometrists rely on TempSure Envi to treat patients with dry eye disease. Usually caused by Meibomian Gland Disease or MGD, the combination often makes a person look tired. In addition to dealing with uncomfortable symptoms, this causes bags to form beneath the eyes.
Because TempSure Envi is a gentle and safe treatment, it’s ideal for giving people with dry eye disease from MGD a fresher appearance.
How Does TempSure Envi Work?
This treatment uses a radiofrequency that gently and safely heats the skin for a specific amount of time. The body naturally reacts by producing new collagen. Because the new fibers are tighter and denser, they fill in voids in the form of lines, wrinkles, and cellulite. It also diminishes bagginess associated with dry eye disease from MGD.
Benefits of TempSure Envi
Experts in the field of aesthetics can use TempSure Envi on many different parts of the body. At the same time, optometrists can use it on patients with dry eye disease.
Most people notice an improvement after just one session. Initially, their skin looks more toned and feels tighter. With each treatment, new collagen will continue to grow. To achieve optimal results, most individuals need at least four sessions.
Additionally, the Food and Drug Administration (FDA) approved TempSure Envi as a viable treatment for all the reasons mentioned. Specifically, it stated that even as a non-invasive solution, TempSure Envi is capable of rejuvenating a person’s appearance, and with no downtime.
Keep in mind that everyone responds somewhat differently. It may take a few more sessions to see desired results. However, most enjoy tighter and more youthful-looking skin for about six months after just four sessions.
To maintain their appearance and continue the cycle of collagen growth, people can have additional TempSure Envi treatments done without any problem. Usually, people have much the same experience. That consists of redness that appears in roughly a day or two. However, it goes away quickly.
The Bottom Line
TempSure Envi is an FDA-approved and non-invasive treatment that helps people achieve tighter and more toned skin. Additionally, it doesn’t cause any real side effects, and it doesn’t involve any recovery time. Many individuals who opt for this treatment can have it done during their lunch break and return to work with better looking skin appearance.
MiSight
Over the years, contact lenses have evolved. A new product called MiSight is giving children a new and improved option. MiSight lenses effectively treat myopia, otherwise known as nearsightedness.
Myopia
Myopia is the medical term used for nearsightedness. Of all correctable visual impairments, myopia ranks number one. With this condition, the eye grows too long from the front to the back. As a result, images don’t focus on the retina. Instead, they focus at the front of it. With this refractive error, individuals can see things up close without any problem but everything at a distance appears blurry. Over time, myopia in children typically worsens. This refractive error puts them at risk of developing other problems. For example, they’re more prone to having premature cataracts and detached retinas as an adult.
To treat this condition, most opt for prescription eyeglasses or contacts. Although MiSight Lenses work similarly to conventional lenses, they’re unique.
Benefits of MiSight Lenses
These contacts slow the progression of myopia in children between the ages of eight and 12. Even more exciting, they slow the progression by as much as 59%. For instance, if an ophthalmologist or optometrist diagnoses a child with nearsightedness and predicts a diopter of -8.00, MiSight contact lenses can reduce that to about -3.50.
As the only contact lens on the market capable of doing this, the Food and Drug Administration (FDA) fully approved them in 2019.
Another benefit of wearing MiSight contacts over traditional lenses is their soft lens. Especially for younger wearers, they provide optimal comfort.
Also, an individual only wears them once before discarding them. It’s important to note that these contacts aren’t made for overnight wear. For that reason, users need to remove them from the eyes and discard them at the end of each day.
Uniquely Designed
MiSight contact lenses work because of their unique design. After placing them in the eyes, one portion of the lens corrects the refractive error of nearsightedness. This allows the individual to see things at a distance. Another part of the lens focuses some light in front of the retina. This element of the design causes the progression of myopia to slow down.
MiSight contact lenses are ideal for both slight and severe cases of myopia. Even some of the other more advanced contacts can only correct around 1.00D. For short-sight prescriptions, an optometrist can prescribe MySight contacts as low as -0.250 and as high as -6.00D.
Correcting Vision Safely and Effectively
MiSight contacts are not ordinary lenses. Rather, they treat the myopia refractive error so that children can see better and prevent their vision from becoming worse. They also reduce the risk of additional eye and vision-related problems. Everything combined makes these contact lenses a perfect choice for treating myopia in children.
Overview of Visian ICL
Visian ICL, or “implantable Collamer lens” is an alternative procedure for patients who may not be ideal candidates for Lasik or other alternative corrective eye surgery. Visian ICL is typically used for patients who do not want to remove portions of their cornea, have thin corneas, or that have excessively high levels of nearsightedness (myopia).
This procedure makes a small incision and then implants a personalized prescription lens over the cornea to allow for corrected vision. If your vision then changes due to aging or other natural processes, the lens can be replaced by another lens with an updated prescription.
Who is a Good Candidate for ICL?
Typically, patients that would benefit from ICL are between the ages of 21-45. This age represents a slight increase from the base age of 18 for Lasik. This procedure is also not well suited for geriatric or elderly individuals. Patients may also have mild or severe myopia, and they have a prescription that has been relatively unchanged. While the age requirements are more stringent for ICL than Lasik, there are other less stringent qualifications. This means that even if you aren’t an ideal candidate for Lasik, ICL could be a good option for you.
Performing the Operation
ICL is considered an outpatient operation and only takes about 30 minutes to complete. This means that you will be in and out of your chosen facility on the same day. Patients are given some numbing drops for their eyes and individuals that are more hesitant or uncomfortable may also be given a sedative.
The surgeon will make several micro-incisions in the eye to insert and place the lens. When the lens has been inserted, it will be unfolded, and the edges of the lens will be placed behind the iris. After this is completed, the operation is considered complete. Your physician may give you some eye drops for postoperative care and then send you home. There may be a follow-up appointment scheduled 24 hours later.
Post-Operation
After your operation, you will be required to have somebody else drive you home. Anytime that you have an operation that may impair your vision or ability to operate a vehicle, you should plan to have somebody else drive you home. Surgery results are typically noticeable 24 hours after the operation.
Recovery time is minimal, and some patients experience mild discomfort or a gritty feeling in their eyes. Your doctor may require you to stay out of the swimming pool and avoid activities that make you heavily perspire because when sweat gets into your eyes, it may aggravate the micro incisions and cause additional discomfort.
While there are some potential complications both during and after the operation, they are typically minimal. The chances of impairing your vision or causing long-term damage are very low with this operation, however, you should make sure to talk about potential side effects with your physician. If you experience any abnormality, you should seek medical attention immediately.
Corneal Refractive Therapy
Corneal refractive therapy, also known as CRT, is a simple, painless treatment for refractive eye errors like myopia and has two core benefits. First, it can be used to help patients see clearly during the day without using glasses or contact lenses, giving them the freedom and flexibility that they need to live life to the fullest. Second, CRT has been shown to help slow the progression of myopia, keeping prescriptions under control and potentially reducing the likelihood of patients developing serious eye health problems associated with high myopia in the future.
Here’s everything that you need to know about corneal refractive therapy and what it means for you.
Understanding refractive eye problems
Refractive eye problems like nearsightedness, farsightedness and astigmatism are extremely common, with nearsightedness – also known as myopia – being the most common of all. Patients with myopia can see nearby objects clearly, but those further away become progressively more blurred. Refractive eye errors occur when the shape of the clear dome covering the front part of the eye, called the cornea, impair the light-bending and focusing process in your eyes. This leads to the light ending up in the wrong place inside the eye, and the message that is sent to our brain from our eyes is muddled, causing blurred vision.
What is corneal refractive therapy?
Corneal refractive therapy was initially developed as a treatment to correct and slow the progression of nearsightedness. However, it has also been found to be effective at controlling other refractive errors, including farsightedness, astigmatism and an age-related refractive condition called presbyopia.
CRT is a non-invasive, painless and straightforward method of correcting patient vision so that they don’t need to wear contacts or glasses, and they don’t need laser vision correction surgery to see clearly. CRT uses special contact lenses that are worn overnight and apply light pressure to the cornea in order to reshape it so that light is refracted correctly, and the image sent from the eyes to the brain is clear. The cornea is able to retain this new shape even after the contact lenses are removed the next morning, meaning that you can continue to see clearly for several hours. The more consistently you wear your CRT lenses overnight, the longer your eyes will learn to retain their new shape and eventually, patients can enjoy up to 48 hours of clear vision without using prescription lenses. However, the effects aren’t permanent so if you stop wearing the lenses, your vision will gradually return back to normal over the course of a few days.
Slowing the progression of myopia with corneal refractive therapy
Another key benefit of CRT is that it can actually help to slow the progression of myopia. Most people who are nearsighted find that their eyesight gets progressively worse as they get older. This deterioration may not be rapid, but it can end in patients requiring high prescriptions. Studies have found that patients who have high myopia are more likely to develop serious eye problems in the future, including glaucoma, macular degeneration, cataracts and a detached retina. Regular use of your corneal refractive therapy lenses could help keep your prescription stable and lower your risk of developing these problems.
Am I a candidate for corneal refractive therapy?
You may be a candidate for corneal refractive therapy if you:
Have a myopia prescription within specific parameters
Have a prescription for hyperopia, presbyopia or astigmatism within specific parameters
Have stable vision, which means that your prescription hasn’t changed during the last two years
Are not a suitable candidate for laser vision correction
Have a job that makes it impractical or unsafe to wear glasses or contact lenses
Enjoy hobbies that make it impractical or unsafe to wear glasses or contact lenses
Have healthy eyes and are generally in good health
For more information, please contact our friendly and knowledgeable team today.
Am I a candidate for LASIK?
If you already rely on wearing glasses or contact lenses to be able to see clearly, you may be frustrated with the effect that they have on your life. Regular vision tests, finding glasses to suit your face shape, having to remember to take eyeglasses with you wherever you go, prescription sunglasses, fiddly contact lenses… the list of inconveniences associated with conventional ocular solutions is extensive.
LASIK is a modern, minimally-invasive procedure that can substantially reduce or eliminate your need to use eyeglasses or contact lenses, allowing you to enjoy life without limitations or inconvenience. The popularity and success of LASIK laser eye surgery have helped to make it the number one elective surgery across the globe.
Candidacy for LASIK
LASIK has an extremely high success rate. According to the American Society of Cataract and Refractive Surgery, 96% of patients achieve 20/20 vision or better. However, it’s high success rate doesn’t make LASIK automatically the right solution for everyone.
Candidacy for LASIK is assessed by our doctors on a case by case basis so that you be certain that whatever treatment is recommended for you, it will give you the very best opportunity to improve your vision. During your consultation, our doctors will perform a thorough examination of your eyes and vision, ask you about your general health and talk you through both the procedure and aftercare.
The general guidelines for LASIK candidacy state that patients must:
be at least 18 years of age
have had stable vision with no prescription changes for a minimum of 12 months
have a current prescription for eyeglasses or contact lenses that falls between specified parameters (Our doctors will be aware of what these parameters are)
have no significant medical or eye-related problems such as glaucoma, macular degeneration or diabetic retinopathy
have no history of corneal disease
not be pregnant or nursing at the time of the procedure
Lens Technology
Thanks to the advancement of lens technology, glasses lenses are no longer a single, one size fits all solution. There are a variety of different lens types that can be used in glasses, giving patients greater flexibility and control over their vision than ever before.
Single Vision Lenses
Also known as monovision lenses, these lenses are designed to correct the wearer’s vision at just one distance, and have a single prescription covering the entire surface of the lens. They are most often recommended for people who are either nearsighted (myopia) or farsighted (hyperopia) and who need glasses for a specific activity, such as driving or reading.
Progressive Lenses
Progressive lenses are multifocal lenses that can correct a patient’s vision at different working distances, ranging from far distance to reading distance. However, rather than designating different areas on the lenses for different distances with visible lines separating them, progressive lenses have a gradual change so that the wearer can smoothly transition from one lens power to another.
Bifocal and Trifocal Lenses
As you may have guessed from the name, bifocal and trifocal lenses have either two or three lens powers depending on which type you choose. Bifocal lenses support distance vision in the top half of the lens, and near vision in the lower half. Trifocal lenses support distance vision in the top third of the lens, intermediate vision in the middle segment and near vision in the bottom third. Whichever variety you choose, you will see visible lines separating each segment.
Bifocal and trifocal lenses are recommended for patients who are near or farsighted, and those who develop presbyopia, which is the natural hardening of the eye lens, that occurs as we get older. Presbyopia makes it harder for the lens of the eye to adapt to focus at different distances.
Multifocal Lenses
Multifocal lenses are the alternative name given to bifocal, trifocal and progressive lenses.
Computer Lenses
Computer lenses are prescription lenses that are specifically designed to be worn when doing computer work. This is because they place the optimum lens power for viewing your computer screen exactly where you need it – which is closer than intermediate vision, but further away than reading material is usually held. Wearing computer lenses can significantly reduce the negative effects caused by the high visual demands of computer work, including blurred vision, redness, dry eyes, double vision and dizziness.
Transition Lenses
Also known as photochromic lenses, transition lenses are a special type of lens that darken when in the sunlight and lighten when in softer light or the dark. This versatility gives the wearer the convenience of being able to move between different environments without needing to change their glasses. This makes them extremely cost effective and prevent the wearer from needing to take multiple pairs of glasses out with them. Transition lenses also filter out many of the harmful UV rays that are emitted from the sun, helping to keep eyes healthy too. They are ideal for people who spend a lot of time going between inside and outside, or who work outside in varying weather conditions.
Blue Light Lenses
Blue light lenses are specially crafted lenses that contain filters that block out much of the artificial blue light that is produced by digital devices like computers, smartphones and tablets. Natural blue light is actually good for balancing our sleep-wake cycle, boosting our mood and enhancing our cognitive abilities so that we can function better day to day. However, too much blue light, especially from artificial sources, can have the opposite effect. Many people who fail to use blue light lenses can go on to develop digital eye strain, which produces symptoms like eye fatigue, dry eyes, blurred vision, headaches and more. Blue light lenses are recommended for anyone who spends a lot of time working on a digital device.
Polarized Lenses
Polarized lenses are used to reduce eyestrain and improve the quality of vision in patients on especially sunny days, making them ideal for anyone who spends a lot of time outdoors. They can do this because they have a special filter that blocks some of the light from passing through the lens. Vertical light is allowed to pass through, while horizontal light, such as that which bounces off of water and can be blinding, is blocked. Polarized lenses are most often used in sunglasses since they are worn outdoors, and the wearer also needs to protect their eyes from UV damage.
Still have questions about which lens is right for you? Contact us to schedule an eye exam or an appointment to evaluate your individual needs.
How Exercise Benefits the Eye
It is common knowledge that exercise plays a critical role in healthy living. Exercise can help improve energy levels, lower blood pressure, aid in weight loss, helps to build muscle and so much more. But one benefit of exercise that is not as well known is the profound impact on your eyesight.
Based on recent research, eye conditions are usually a direct result of a health issue such as high blood pressure, diabetes, high cholesterol level, etc. While some of these diseases are unavoidable, exercising regularly can definitely help in the prevention of these diseases and in doing so, help keep the eyes healthy. In addition to physical exercise, there are even some eye exercises that can be done to keep your vision healthy. Some examples are focusing on certain points, rolling your eyes in different directions, writing with the eyes, etc.
Cataracts and Exercise
According to a study in 2003 and another in 2006, a relationship was discovered between an increase in exercise and a decrease in cataract. It emphasized that there is a greater chance for cataract if there is an absence of physical activity. This implies that taking a light walk or jog around your house or on a field track consistently can contribute to the fight against cataracts.
Macular Degeneration and Exercise
According to one study, exercising three times or more on a weekly basis reduces ones’ chances of developing exudative macular degeneration. Exudative macular degeneration occurs when blood vessels grow beneath the retina that are not needed and then leak fluid and blood into the eyes.
Glaucoma and Exercise
One major cause in the development of glaucoma is an increase in ocular perfusion pressure. Very light exercises like jogging or walking at least three times weekly helps to reduce the intraocular pressure and improves the flow of blood to the optic nerve and retina.
The benefit of eye exercises
Protects against dry eyes. Eye exercises help maintain and improve the fluid level in the eyes, thus eliminating the probability of dry eyes because as the eyes are being exercised say by rotation, there is the tendency that fluid is produced.
Reduces eye strain and tension. Exercising the eyes daily helps in reducing the strain and tension that has been placed on the muscle. Exercises like rolling the eyes and writing with the eyes help in the contracting and relaxing of the eye muscles. Long hours of study or use of a computer can cause blurry vision, but through exercise, clarity can be achieved by eliminating tension and unnecessary pressure.
Make the eye muscles flexible. Exercises like shifting and swinging the muscles of the eyes help promote flexibility in the muscles of the eyes. Just like exercise helps the body muscles, the same thing applies to eye exercises.
Benefits of LASIK
LASIK is the number one elective surgical procedure today, and more than a million Americans have had the procedure since its inception. The main reason for its popularity is the many benefits that it offers, including minimizing or in some cases even eliminating the need for the patient to use eyeglasses or contact lenses after the procedure.
Let’s take a look at why LASIK is taking the ocular world by storm.
Better vision
Clearly, the biggest reason for choosing LASIK is improved vision. While some patients have relatively mild problems with their eyesight, others experience major disturbances in their vision that makes functioning day to day almost impossible without the use of visual aids. LASIK can dramatically improve the quality of your vision, reducing the need to wear visual aids, or in some cases, completely eliminating it.
A good investment
Eyesight is also notoriously inconsistent, with the majority of people finding that their vision marginally improves or deteriorates with each visit to their optician. When this happens, it is necessary for the optician to recommend a different prescription, and this means expense as the patient finds themselves purchasing new eyeglasses or contacts to reflect their new visual requirements.
Although there is no guarantee that you will be able to completely prescription-free after LASIK, most patients find that eyesight is so improved that any changes to their prescription are much less frequent.
Eyeglasses and contacts are known for being fiddly and fragile, and the need for maintenance and replacements are a common complaint. However, with less need for such devices, the cost of caring for them is also reduced.
A short, painless procedure
LASIK surgery can be performed in one, very short procedure. You should expect to spend around 30 minutes in the surgery suite, but the actual time it takes can be as little as 10 minutes – for both eyes! The remainder of the time will be spent preparing you and ensuring you are comfortable afterward. The entire process is carried out after anesthetic drops have been placed into your eyes, so you can rest assured you will feel absolutely no pain throughout. However, if you are particularly anxious about the process, it may be possible to be given a sedative to help you relax.
Cosmetic Services
We all want to look our best and in the last decade, we have seen a significant increase in the number of people seeking cosmetic services in order to enhance their appearance. With our eyes being our most distinguishing feature, we want to make the most of them. Thankfully there is now a range of cosmetic services that can help to rejuvenate our eyes and the area around them to keep them fresh, young and wrinkle-free.
Let’s take a look at some of the services on offer.
Pigment removal
The brown pigment spots that appear on the face are often referred to as age spots and are a result of sun exposure. With age, the repeated exposure to UV rays causes melanin, a compound that is responsible for pigmentation and protecting the skin begins to clump together to form an area of hyperpigmentation. Whilst they aren’t any cause for concern, many people feel that they look unsightly. Luckily, there are a number of different treatments that you can get to remove them including topical creams, laser therapy, and chemical peels.
If you are suffering from darker pigmentation then we strongly recommend that you make an appointment with a qualified dermatologist who will recommend the best course of treatment for you, based on your specific needs.
Blephex
Our eyes are extremely delicate, yet they can be subjected to harsh conditions and other environmental factors that affect their health. One of the problems that can affect our eyes is an accumulation of dirt, debris and bacteria on the eyelids. This can cause a range of issues, including stopping tear film from reaching the eyes and being properly dispersed over their surface – which is necessary to keep them healthy and comfortable. Fortunately, a new solution called BlephexÔ can help.
What is BlephexÔ?
BlephexÔ is a handheld electro-mechanical device that is applied to the margins of the eyelids with the purpose of cleaning them and improving the effectiveness with which tear film flows onto the surface of the eyes.
BlephexÔ has a disposable, surgical-grade sponge tip which rapidly oscillates to create a cleaning action. Before the sponge tip is placed onto the eyes, it is soaked in a gentle exfoliating solution. This solution provides soft abrasion to help remove dead skin cells and debris that could be irritating the eyes and interrupting tear film progression. The BlephexÔ device is manually applied to the eyes and moved gently across the eyelids, with the entire, painless process taking approximately 6 to 8 minutes per eye. A different sponge is used on each eye, ensuring that no bacteria is passed between them. After the procedure, patients are given instructions on how to maintain the cleanliness of their eyelids with daily/nightly eyelid hygiene at home.
Most patients experience a significant improvement in tear film production and dispersal, and a reduction in unpleasant symptoms that they may have been experiencing within 48 hours of their treatment. While a single treatment is normally enough to produce excellent results, many patients are advised to have BlephexÔ every 4-6 months.
What conditions can BlephexÔ help with?
BlephexÔ can be used to clean the eyelids at any time, and people who suffer from dry eyes or eye allergies may find it is particularly beneficial for helping to reduce the symptoms that they experience. It can also be combined with Lipiflow – another technological solution – to help counteract the effects of dry eyes.
Unsurprisingly, BlephexÔ is particularly recommended as a treatment for an eye condition called blepharitis. Blepharitis is characterized by the inflammation of the eyelids, which causes them to become red, swollen and itchy. Although the condition is not usually serious, it can lead to further problems if it isn’t treated.
Symptoms of blepharitis include:
Sore eyes
Itchy eyes
A gritty, irritated feeling affecting the eyes
Redness
Flakes or crustiness around the roots of the eyelashes
Eyelids that stick together when you wake up in the morning
If you are suffering from the symptoms of blepharitis, dry eyes or eye allergies and feel that you would benefit from BlephexÔ treatment, please contact our team to schedule a consultation appointment.
Visual Field
Visual field testing is an important part of most standard comprehensive eye exams. Also sometimes known as perimetry testing, Visual field testing is a method to measure the entire scope of vision of an individual, including their peripheral/side vision.
The importance of visual field testing
Visual field testing is one of the most effective diagnostic treatments in the detection of glaucoma. This is because when patients are affected by glaucoma, it is usually the peripheral vision that is affected by their condition first. However, it can also be used to detect central or peripheral retinal diseases, eyelid conditions such as drooping, optic nerve damage and conditions that affect the visual pathways from the optic nerve to the area of the brain where this information is processed into vision.
Visual field testing is also an important part of monitoring for people who are considered to be at risk for vision loss from disease and other problems, including those who have been diagnosed with the following:
Multiple sclerosis
Hyperthyroidism
Pituitary gland disorders
Central nervous system problems (such as a tumor that may be pressing on the brain)
Stroke
Diabetes
High blood pressure
What to expect from visual field testing
There are a variety of methods that can be used to perform visual field testing, including:
Static automated perimetry. This is where a machine is used to quantify how well the patient is able to detect flashing lights of varying size and brightness in different areas of their visual field, while they concentrate on a central point. The patient responds by pushing a button when they see the light.
Kinetic perimetry. This involves points of light that are fixed in size and intensity and are presented along the patient’s peripheral vision, before being gradually moved inwards to determine their field of vision.
Visual field testing is non-invasive, painless and doesn’t require patients to have their eyes dilated. The results, which are usually presented in a series of charts, are digital and sent directly to your eye doctor for interpretation. Depending on the outcome of your results, you may be recommended for further diagnostic testing which could include blood tests. If you have been diagnosed with glaucoma, you will probably be recommended to have several visual field tests each year, which will help your eye doctor to monitor the progression of your condition and recommend treatments to slow it.
If you would like more information about visual field testing, or if you have concerns about your peripheral vision, please don’t hesitate to schedule an appointment with our experienced and knowledgeable eyecare team today.
Myopia Management
Myopia is a very common issue throughout the world. Approximately 1/3 of the population in the United States have the condition and over 90% of several East Asian countries suffer from myopia. While myopia may seem like such a common condition that it shouldn’t be cause for concern, it is actually associated with several very serious conditions that can threaten one’s ability to see.
What is Myopia
Myopia, more commonly known as nearsightedness, is a condition where individuals are able to see objects that are close to them but may have difficulty distinguishing things at a distance, such as road signs or leaves on a tree. These individuals often squint at objects that are further away to try and help bring them into focus.
Currently, there is no known cure for myopia and recent studies suggest that the more advanced your myopia gets, the more serious the effects can be on your vision. This has led eye professionals to look for ways to slow the progression of myopia in children and young adults as the eyes typically change more rapidly during this time and slowing down myopia progression during these years has a huge payoff.
Types of Myopia Control
There are a few different treatments for myopia that have proven to be effective in a number of studies. Of course, to ensure you find the most effective choice for you, be sure to visit with your eye doctor so they can review your case and recommend the best options for you.
Ortho-K | Ortho-K or Orthokeratology is one practice being used to slow down the progression of myopia. Ortho-K utilizes a special rigid gas-permeable contact lens that is placed into the eyes just before you go to bed. This hard lens helps to gently hold your eye in the proper shape throughout the night. Then when you wake up in the morning and remove the lenses, your eye continues to maintain that shape. This means that people who are nearsighted can see clearly throughout the day, even without wearing contact lenses or glasses. This approach is often preferred for athletes or other active individuals.
Atropine Eye Drops | One of the thoughts about the progression of myopia, is that it is associated with eye strain. The additional stresses that are placed on the eye when straining push the eye further out of its proper shape. Atropine eye drops are specifically designed to help stop the eye from straining and help the muscles relax. Atropine is similar to the eye drops that are used when you get your eyes dilated but lasts throughout the entire day rather than just a few hours. Atropine dilates the pupil of the eye and prevents them from closing too tightly and limiting your vision. This treatment has been shown to be especially effective in slowing the progression of myopia in children.
Multifocal Eyeglasses and Contact Lenses | These specialty contact lenses are designed to help reduce strain on the eyes. They have shown great success at slowing the progression of myopia over a three-year period when compared with individuals who wore a standard prescription lens.
Overview
If you notice that your child is having a difficult time seeing objects that are far away, contact us today to schedule an appointment. Many parents notice changes in their children with their behavior or grades at school, their ability to play sports, or that they may even be pulling back from playing with friends. Treating myopia as quickly as possible can help to reduce your child’s chances of developing a serious eye condition that can threaten their ability to see the world around them. Call today and schedule an appointment to see how we can help your child.
Low Vision
Low vision is a term for conditions that result in reduced sight and cannot entirely be corrected with eyeglasses, contact lenses, medicines or surgery. Several eye diseases or conditions can cause low vision and here we will discuss the four most common causes of low vision and their risk factors.
Macular Degeneration
Macular degeneration is a disorder that affects the retina, which is the light-sensitive tissue lining the inside of the eye. Within the retina, the area responsible for sharp central vision (called the macula) deteriorates, causing blurred vision. This can cause a blind spot in the central area of vision, which leads to low vision.
There are two types of macular degeneration – non-exudative (dry form) and exudative (wet form). The dry form usually progresses slowly, while the wet form causes more rapid and severe vision loss due to abnormal blood vessels developing under the macula and leak fluid and blood. The biggest risk factor for macular degeneration is age. Other risk factors include genetics, race, smoking, and high blood pressure.
Diabetic Retinopathy
Diabetic retinopathy is a diabetes complication that affects the eyes. High blood sugar levels cause damage to blood vessels in the retina. These blood vessels can swell and leak (called macular edema). Sometimes they close, stopping blood from passing through (called macular ischemia). At first, diabetic retinopathy may cause no symptoms or only mild vision problems. However, over time, it can severely damage the retina, leading to low vision. Anyone who has diabetes can develop diabetic retinopathy. The risk increases for those who have had diabetes longer, as well as those with poor control of blood sugar levels, high blood pressure or cholesterol as well as those who smoke.
Cataracts
A cataract is a clouding of the lens in the eye that affects vision. This clouding can block the light from reaching the retina at the back of the eye, resulting in a general loss of vision. In some cases, a cataract can be surgically removed. Cataract surgery has a high success rate in otherwise healthy eyes but it is not always possible for people who also have other eye diseases. While the risk of cataract increases as you get older, other risk factors include diabetes, smoking, alcohol use, and prolonged exposure to ultraviolet sunlight.
Glaucoma
Glaucoma is a disease that damages your eye’s optic nerve. Most commonly, this occurs when fluid builds up in the front part of your eye which increases the pressure in your eye, damaging the optic nerve. There are four types of glaucoma: open-angle, normal tension, angle-closure, and secondary.
Eye Emergencies
Eye emergencies cover a range of incidents and conditions such as; trauma, cuts, scratches, foreign objects in the eye, burns, chemical exposure, photic retinopathy, and blunt injuries to the eye or eyelid. Since the eye is easily damaged, serious complications can occur from an eye injury thus, any of these conditions without proper treatment can lead to a partial loss of vision or even permanent blindness. Likewise, certain eye infections, other medical conditions, such as blood clots or glaucoma, and eye problems such as a painful red eye or vision loss that are not due to injury also need urgent medical attention.
Depending on the type of injury, any of the following symptoms may be present:
Bleeding or other discharge from or around the eye
Bruising
Decreased vision
Double vision
Loss of vision, total or partial, in one eye or both
Pupils of unequal size
Eye pain
New or severe headaches
Itchy eyes
Redness or bloodshot appearance
A sensation of something in the eye
Sensitivity to light
Stinging or burning in the eye
One eye is not moving like the other
One eye is sticking out or bulging
Nausea or headache occurring with eye pain (this may be a symptom of glaucoma or stroke).
A black eye is usually caused by direct trauma to the eye or face, causing a bruise resulting from bleeding under the skin. The skin around the eye turns black and blue, gradually becoming purple, green, and yellow over several days. Swelling of the eyelid and tissues around the eye may also occur. The abnormal color usually disappears within 2 weeks.
A blow to the eye can potentially damage the inside of the eye. Trauma is also a common cause of hyphemia, which is blood inside the front of the eye and is often due to a direct hit to the eye from a ball. Besides, certain types of skull fractures can cause bruising around the eyes, even without direct injury to the eye.
A chemical injury to the eye can be caused by a work-related accident, common household products such as cleaning solutions, garden chemicals, solvents, or other types of chemicals. Fumes and aerosols can also cause chemical burns. With acid burns, the haze on the cornea often clears and there is a good chance of recovery. However, alkaline substances such as lime, lye, drain cleaners, and sodium hydroxide found in refrigeration equipment may cause permanent damage to the cornea. It is important to flush out the eye with large amounts of clean water or salt water (saline).
Glaucoma Testing
You might be surprised at how many tests eye doctors use to diagnose glaucoma. A proper diagnosis requires careful evaluation of many aspects of your eye’s health – from eye pressure to cornea thickness to the health of your optic nerve. This article describes how your eye doctor assesses your risk and all the tests needed to properly diagnose glaucoma.
Risk Factor Assessment
Your eye doctor will begin by assessing your risk level for developing glaucoma. This will help determine the frequency and extent of testing needed. Through a family history and medical questionnaire, the eye doctor is looking for the following risk factors:
Over the age of 60
Ethnic background such as African or black Caribbean descent, Hispanic, or Asian
Family history of glaucoma, such as a sibling or parent with glaucoma
History of eye conditions, injuries or surgeries
Prolonged corticosteroid use (eye drops, pills, inhalers or creams)
Chronic conditions that affect blood flow, such as migraines, diabetes, low blood
pressure or hypertensionCurrent or former smoker
If you’ve already had a comprehensive eye exam, your eye doctor will also consider these risk factors:
Eye pressure higher than normal (above 21 mm Hg)
Thin corneas (less than 0.5 millimeters)
Your type of eyesight is also important. People with farsightedness are at a higher risk for narrow-angle glaucoma, a more serious type that can advance quickly. While nearsightedness is associated with open-angle glaucoma, which progresses slowly without any symptoms.
Standard Glaucoma Tests
During a comprehensive eye exam, your eye doctor will always check for glaucoma, regardless of the risk level. This provides a baseline for comparison as you age. There are two tests: tonometry and ophthalmoscopy.
Lumenis Optilight IPL
Millions of people suffer from eye and vision-related problems. For some, the solution is as simple as wearing prescription eyeglasses or contact lenses. However, others face challenges that aren’t as easy to rectify. That’s where Lumenis comes into play.
As a world leader in minimally invasive clinical solutions for both ophthalmology and aesthetic markets, it’s making a significant difference. Not only does Lumenis develop advanced energy-based technologies, but it also commercializes them.
The company continues to find innovative solutions. However, it’s already provided the fields of ophthalmology and aesthetic with remarkable technologies. OptiLight is just one example.
Eye and Vision-Related Solution
The company invented the first and only technology to treat individuals for dry eye disease caused by MGD. Not only is it approved by the Food and Drug Administration (FDA) but also patented. Optimal Pulse Technology (OPT) makes it easier to successfully manage this particular eye disease. Overall, OptiLight is safe, precise, comfortable, and effective.
Managing Symptoms
According to recent statistics, roughly 22% of the U.S. population suffers from dry eye disease along with MGD. That combination leads to an array of uncomfortable symptoms.
Dry eye occurs when a person’s eyes don’t produce adequate tears to keep them lubricated or when tears don’t work the way they should. MGD is a condition that affects the small glands in the eyelid responsible for making the oil layer for tears.
Having to deal with one of these problems is bad enough. However, living with both can prove debilitating for some people. Thanks to OptiLight, people with the two conditions get much-needed relief. Here are the ways this advanced technology helps:
Reduces inflammatory mediators, which, thereby, prevents inflammation
Improves tear breakup time that, in response, decreases osmolarity
Alleviates abnormal blood vessels that commonly cause inflammation
Restores meibomian glands so they function properly
Decreases demodex mites that cause infection and the accumulation of bacteria on the eyelids
What Does OptiLight Consist Of?
As part of this revolutionary system, ophthalmologists and optometrists can select different devices based on their needs.
Patented OPT Handpiece
Not two people have identical faces. Even among twins, facial contours differ, even if slightly. To ensure excellent results, this handpiece allows ophthalmologists and optometrists to customize treatments to cover every curve.
Ergonomic IPL Handpiece
To treat a broader area, Lumenis recommends this option. Patented with SapphireCool technology, it breaks the cycle of inflammation associated with dry eye disease caused by MGD.
Opti-Tip
For maximum energy control, the Opti-Tip focuses light energy on more delicate areas. As with the other Lumenis devices, it’s safe and effective. At the same time, the Opti-Tip is 100% hygienic.
Key Benefits of OptiLight
OptiLight utilizes embedded settings that adhere to strict protocols, making it safe and effective tool.
Additionally, they use Optimal Pulse Technology (OPT), which transforms light-based therapy. As a result, ophthalmologists and optometrists can treat the eyes with absolute precision and control. That’s because while this technology provides optimal energy, it never has spike inconsistencies.
Doctors can treat a patient in just 15 minutes. Specifically for dry eye disease with MGD, it provides an improvement in just four sessions.
The Bottom Line
Lumenis dedicated years to develop OptiLight. Now, eye doctors can incorporate a system into their practice to provide better patient care.
LASIK Co-management
LASIK co-management is an integral part of vision correction surgery that often goes unnoticed. It involves a partnership between your primary eye care professional and your LASIK surgeon. This cooperative approach ensures that you're provided with the best possible care before, during, and after your procedure.
LASIK co-management is the collaborative effort of your eye care team to ensure your vision correction procedure is safe and successful. It's a team approach where everyone plays a significant role in your eye health journey.
The Evaluation Process
The evaluation process in LASIK co-management is thorough and meticulous. It begins with a comprehensive eye examination by your primary care optometrist. This examination is meant to ascertain your eye health status and determine if you're an appropriate candidate for the LASIK procedure.
The evaluation process underscores the collaborative nature of LASIK co-management. Every step is carefully coordinated to ensure your eye health is prioritized and that you're receiving the best possible care.
The Importance of Consultation in LASIK Co-management
Consultation is a crucial aspect of LASIK co-management. It allows for patient education, addressing concerns and questions, and establishing a clear understanding of the expected outcomes.
During the consultation phase, your optometrist will explain the results of your eye examination and how it relates to your suitability for LASIK surgery. They will also discuss the risks and benefits of the procedure, giving you a balanced perspective to make an informed decision.
The consultation with your LASIK surgeon will delve into the specifics of the operation, including the technology used, the surgical process, and the anticipated recovery timeline. Having the opportunity to consult with both your optometrist and your surgeon ensures that all your concerns are addressed, allowing you to proceed with confidence.
The Role of Communication
Effective communication is the backbone of successful LASIK co-management. It facilitates a seamless transition from your optometrist to your surgeon, creating a cohesive care plan that's centered around your specific needs.
This communication is not just between healthcare providers but also involves the patient. Regular updates on your progress, detailed explanations about each stage of the process, and addressing any concerns or questions you may have are all essential parts of the communication process.
Post-care in LASIK Co-management
Effective post-care in LASIK co-management is crucial in ensuring a successful outcome and speedy recovery. Post-care involves monitoring your healing progress, managing any discomfort or side effects, and ensuring that your vision is improving as expected.
Your optometrist plays a key role in this post-care. They will schedule follow-up visits to check your eyes and ensure they are healing correctly. They will also provide guidance on activities you should avoid and actions you can take to promote healing.
Additionally, if there are any complications or concerns, your optometrist is your first point of contact. They will liaise with your surgeon to address these concerns, demonstrating once again the importance of the collaborative approach in LASIK co-management.
The Benefits of LASIK Co-management
There are many benefits of LASIK co-management. First, it provides a comprehensive approach to your eye care, combining the expertise of your optometrist and your surgeon. This ensures that you're receiving the most thorough care possible.
Second, LASIK co-management creates a seamless patient experience. Your care transitions smoothly from your optometrist to your surgeon and back again. This eliminates any confusion or stress that can often come with navigating healthcare systems.
Finally, LASIK co-management provides continuity of care. Your optometrist, who is already familiar with your eye health history, remains involved in your care throughout the LASIK process. This continuity not only enhances your comfort level but also contributes to a better overall outcome.
Begin Your Journey to Clear Vision with LASIK Co-management Today
LASIK co-management represents the gold standard in vision correction procedures. It leverages the combined expertise of your optometrist and your surgeon, creating a streamlined, cohesive, and patient-centered approach to your care.
From your initial evaluation to post-operative care, every step of the process is carefully coordinated to ensure your safety, comfort, and the success of your procedure. And with the myriad benefits of LASIK co-management, you can approach your vision correction journey with confidence and peace of mind.
If you're considering LASIK surgery, choose a provider that offers LASIK co-management. It's a proven approach that puts your needs at the center and prioritizes your eye health at every step.
Common Eye Disorders Explained
People will often experience some type of eye disorder during the course of their lives. While the majority of these are minor and don’t require treatment, even minor problems can have significant adverse impacts on your vision, and you should seek the guidance of a licensed medical professional.
We’ve compiled some of the most common eye disorders, their causes, and treatments below. This guide is meant to be educational and not all of the disorders listed below require medical attention, but if you are concerned, you should contact your medical provider immediately.
Eyestrain
Eyestrain is a prevalent eye disorder. Most people have experienced this at one time or another. This optical issue can be caused by placing excessive strain on the eyes. It often occurs when reading, viewing a screen or driving for too long. The eyes may begin to feel tired, or a mild burning sensation can occur. Simple rest is often enough to correct this issue. However, if you continue to feel discomfort for a few days, its time to visit your doctor.
Eye Redness
Eye redness can often be a minor issue that is caused by the inflammation or irritation of blood vessels near the eye’s surface. This can be caused by an irritant, lack of sleep, or allergies. If the redness in your eyes is linked to some type of traumatic injury, you should see a doctor. Typical treatments for this condition are eye drops to help lubricate the eye, resting your eyes, or taking medication to treat your allergies. Eye redness can also be a warning sign for conjunctivitis, pink eye, or sun damage. These conditions should receive medical treatment from a licensed professional.
Night Blindness
Some people find that they have difficulty navigating in darker areas like movie theaters, dark rooms, or driving at night. Several possibilities could lead to night blindness. Some may have been born with this condition, or it could be the result of a degenerative retina. These issues cannot be resolved by a medical professional. However, night blindness can also be caused by nearsightedness, vitamin A deficiency, cataracts, or keratoconus. All of these issues can be corrected by a doctor.
Strabismus (Crossed Eyes)
Crossed eyes are not a condition that you can fix by yourself. This issue is seen in the eyes not properly lining up with each other. However, an optometrist may be able to help correct this issue, so it’s worth scheduling an appointment.
Nystagmus (Shaky Eyes)
Nystagmus is the constant shaking of the eyes of which the patient has no ability to control it. Medical professionals have several options for treatment at their disposal. Sometimes vision therapy is enough to strengthen the muscles and correct the issue. If this doesn’t work, surgery can also correct the problem. Your doctor can discuss your best options with you.
Colorblindness
Red and green color blindness is the most common form of colorblindness, although other types may affect your ability to see different color combinations. Color blindness is caused because the eyes lack the appropriate “cones” that help to interpret and differentiate these colors. This makes certain colors appear identical to colorblind individuals. Very severe forms of colorblindness only allow individuals to see shades of gray, but this is very rare.
While there is no current treatment for the correction of color blindness, special contact lenses or eyeglasses can be prescribed to help.
Uveitis
This condition is the inflammation of the uvea. There are several potential causes of uveitis that can be very serious, but uveitis is an umbrella phrase that covers all causes that create inflammation of the middle layer of the eye.
Some of these causes can be compromises of the immune system, like AIDS, rheumatoid arthritis, or ulcerative colitis. If you have light sensitivity, blurred vision, eye pain, and eye redness that lasts more than a few days you should see your eye care professional.
Knowing When to Get Help
Your eyes are a sensitive and critical organ for your health and small injuries or damage to your eyes can have lasting effects. For this reason, if you sense that something is wrong with your eyes, it’s always a good idea to visit your eye care professional. Additionally, make sure to get your regular annual eye exams which can help detect any issues that your eyes may be having and assure that you get the appropriate care more quickly.
Pink Eye
When you were a kid, did you experience your eyes become reddish and all of a sudden, someone close to you was also suffering from it? Your eyes, as well as those who contracted it, got itchy and swollen, right? Then it must have been that you were suffering from pink eye.
Pink eye is well known as conjunctivitis and it is the infection or inflammation of the conjunctiva or the transparent membrane that serves as a covering for the white part of the eye called the sclera that lines the eyelid. In addition to inflammation, there is usually tearing in the eyes that emits a sticky discharge which develops into a crust while one is sleeping, making it difficult for the patient to open their eyes in the morning.
One thing about the pink eye, which could affect one or both eyes, is that it is highly contagious. While it is more common in children, adults can also be victims of this eye condition. Here are the 3 major causes of pink eye:
Bacteria
Streptococci and staphylococci are bacteria types that are most responsible for pink eye. However, chlamydia and gonococci can also cause pink eye. It is accompanied by serious eye pain, itching, swelling, redness, and discharge. The spread of bacterial pink eye is usually as a result of using personal items of infected parties, such as makeup or makeup tools that have been infected with bacteria or putting dirty hands in the eyes. If not treated, it can last for more than 10 days, but if treated, it should resolve in less than 3 days.
Allergies
Pink eye caused by allergies is followed by serious itching and tearing of the eyes. Pain is minimal, but it typically comes with quite a bit of discomfort. Most of the time, pink eye is accompanied by sneezing or coughing. Allergens that trigger pink eyes include grass, dust, pollen, mold, and ragweed. Allergy based pink eye is not usually contagious.
Viruses
Viruses such as the adenoviruses and herpes virus are the most common causes of pink eye. When a virus is the cause, there is usually a lot of teary discharge accompanied by nasal congestion, puffy eyelids, runny nose, and sharp pain. It is usually contracted from cough and sneeze droplets from an infected individual. It can take as long as 2 weeks to treat depending on the seriousness of the infection.
General Symptoms of Pink Eye:
Itchy eyes
Redness of the sclera
Pain
Watery discharge
Swollen eyelids
Hazy or blurry vision
Oversensitivity to light
Prevention
The best way to prevent pink eye is by practicing good hygiene which includes:
Avoid putting dirty hands in your eyes
Make it a habit to wash your hands often
Avoid sharing towels and other personal items
Do not use dirty items
Changing your pillow cover regularly
Do not leave a makeup item open for too long
Avoid sharing makeup items like eyeliners, mascara, etc.
Treatment of Pink Eye
The treatment of pink eye is dependant on its underlying cause. If it is caused by a virus, you just might have to wait for the virus to run its course which could last for about four to seven days. Virus caused pink eye could be easily contracted so it is imperative to try and prevent further spreading. Viruses cannot be cured by antibiotics, but some antiviral drugs could be helpful.
Antibiotics are most effective against pink eye caused by bacteria as they reduce the lifespan of these bacteria and could come in the form of eye drops or pills. Based on the doctor’s prescription, an eye drop should be administered about four to six times daily. It is important you finish using your drugs even after the disappearance of symptoms.
To deal with pink eyes caused by allergies, the allergy should be treated. Once treated, pink eye should disappear. It is also important to avoid allergens as much as possible so as to avoid pink eye.
Whenever the symptoms of pink eye emerge, the best preventive measure is to stay at home until the watery discharge ceases to avoid the spread of the bacteria or virus. You should also visit your doctor immediately to begin treatment. While mild pink eyes generally go away on its own, some of the more serious forms can cause a scar on the cornea.